Understanding the Connection Between Edema and Diabetes
As a person living with diabetes, I have come to learn that there are many complications that can arise as a result of this chronic condition. One such complication is edema, which refers to the swelling that occurs due to the accumulation of fluid in the body's tissues. In this section, we will explore the relationship between edema and diabetes, and how these two conditions are connected.
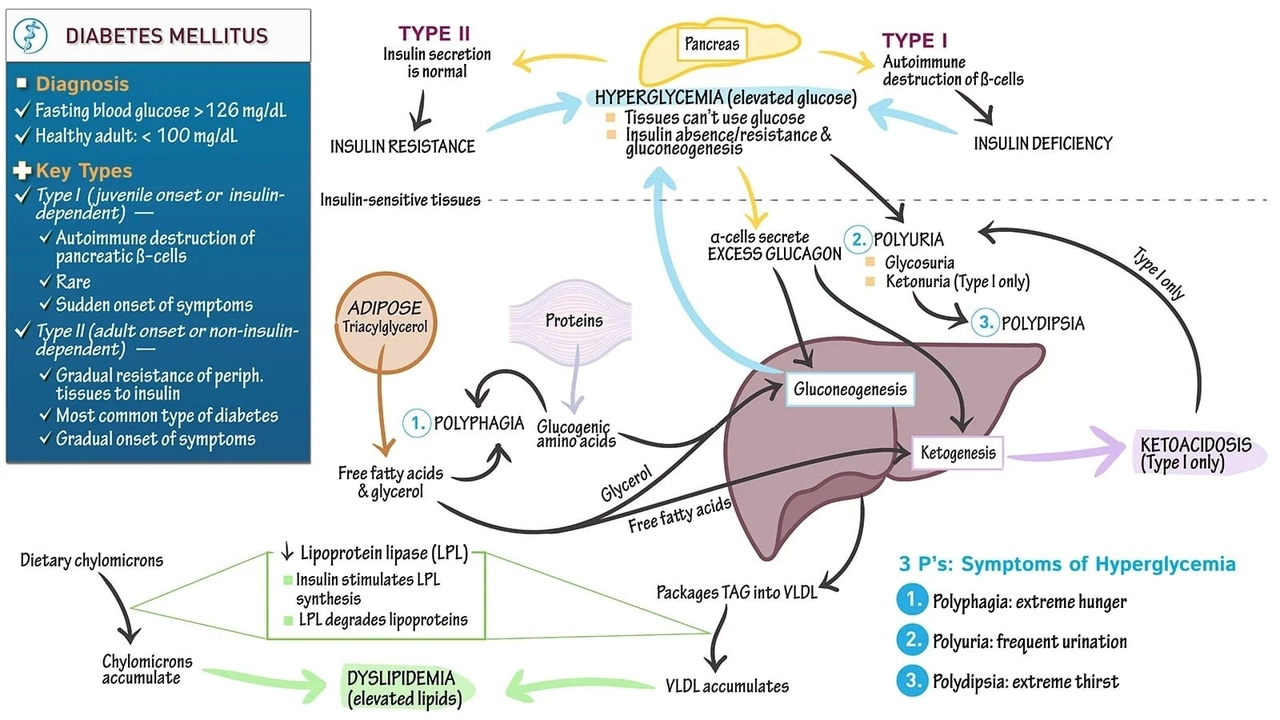
Diabetes affects the body's ability to use and produce insulin, a hormone that regulates blood sugar levels. This can lead to high blood sugar levels, which in turn, can damage blood vessels and nerves throughout the body. One of the ways this damage manifests is through the development of edema, particularly in the lower extremities such as the feet and ankles.
When the blood vessels are damaged, they become more permeable, allowing fluid to leak into the surrounding tissues. This leakage leads to the swelling and discomfort associated with edema. Additionally, nerve damage resulting from diabetes can also contribute to the development of edema, as it can cause a loss of sensation in the affected areas, making it difficult to notice the swelling until it becomes more severe.
Common Causes of Edema in Diabetic Patients
There are several factors that can contribute to the development of edema in individuals with diabetes. It is important for those living with this condition to be aware of these causes, as understanding them can help in the prevention and management of edema.
One common cause of edema in diabetic patients is poor blood circulation. As previously mentioned, high blood sugar levels can damage blood vessels, leading to decreased blood flow in the lower extremities. This reduced circulation can cause fluid to accumulate in the feet and ankles, resulting in edema.
Another factor that can contribute to edema in diabetic individuals is kidney damage. Diabetes can cause damage to the kidneys, impairing their ability to filter waste and excess fluid from the blood. As a result, fluid can build up in the body, leading to swelling and edema.
Lastly, certain medications used to manage diabetes, such as thiazolidinediones, can cause fluid retention and edema as a side effect. If you suspect that your medication may be causing edema, it is important to consult with your healthcare provider to discuss alternative treatment options.
Recognizing the Symptoms of Edema in Diabetic Patients
Being able to recognize the symptoms of edema is crucial for diabetic individuals, as early detection can help prevent further complications and ensure proper management of the condition. Some common signs of edema in diabetic patients include:
- Swelling in the feet, ankles, or legs
- Tightness or stiffness in the affected area
- Pain or discomfort in the swollen area
- Indentations in the skin when pressed (also known as pitting edema)
- Shiny, stretched, or discolored skin
If you are experiencing any of these symptoms, it is important to consult with your healthcare provider to determine the cause and appropriate treatment options.
Complications Associated with Edema and Diabetes
Edema in diabetic patients can lead to a number of complications if left untreated. One such complication is the increased risk of developing skin infections, as the swollen skin is more prone to breaking and becoming infected. Additionally, the reduced blood flow resulting from the swelling can make it more difficult for the body to heal these infections.
Another complication that can arise from edema in diabetic individuals is the development of diabetic foot ulcers. These ulcers can form as a result of the pressure and friction caused by the swelling, and can be difficult to heal due to the impaired circulation and decreased sensation in the affected area.
Lastly, untreated edema can lead to the formation of blood clots in the legs, a condition known as deep vein thrombosis (DVT). These blood clots can be life-threatening if they break loose and travel to the lungs, causing a pulmonary embolism.
Managing Edema in Diabetic Patients
Proper management of edema in diabetic individuals is crucial for preventing complications and maintaining overall health. Some effective strategies for managing edema in diabetic patients include:
- Elevating the affected area, especially during periods of rest
- Wearing compression stockings to help promote circulation
- Engaging in regular physical activity to help improve circulation and reduce swelling
- Reducing sodium intake to help prevent fluid retention
- Managing blood sugar levels to help prevent further damage to blood vessels and nerves
In some cases, your healthcare provider may also recommend medications such as diuretics to help reduce fluid retention and swelling. It is important to follow your healthcare provider's recommendations and to monitor your symptoms closely to ensure proper management of edema and diabetes.
Seeking Medical Help for Edema
If you suspect that you may be experiencing edema as a result of your diabetes, it is important to seek medical help as soon as possible. Your healthcare provider can help determine the cause of the swelling, provide appropriate treatment options, and monitor your condition to ensure proper management.
Remember, early detection and intervention are key for preventing complications and maintaining your overall health. By staying informed about the connection between edema and diabetes, and by implementing appropriate management strategies, you can help ensure a healthier and happier life with diabetes.

20 Comments
Lynnett Winget
May 12, 2023 AT 16:28Hey folks, just wanted to share a little burst of positivity – managing edema while living with diabetes can feel like juggling flaming torches, but remember, each step you take toward better circulation is a victory dance for your body.
Think of elevating those legs as giving them a gentle hug, and compression stockings as stylish superheroes that keep the fluid at bay.
Stay hydrated, keep the sodium low, and let’s celebrate every small win together!
Amy Hamilton
May 13, 2023 AT 09:08It’s truly remarkable how intertwined our vascular health and glycemic control are; each ounce of sugar we tame paves the way for clearer arteries and fewer swelling episodes.
Consider edema as the body’s subtle reminder that something’s amiss, urging us to refine our diet, move more, and perhaps revisit our medication regimen with a clinician.
In the grand tapestry of wellness, these adjustments weave a stronger, more resilient self.
Lewis Lambert
May 14, 2023 AT 00:25Living with diabetes has taught me that edema isn’t just a peripheral nuisance; it’s a signal that the whole circulatory orchestra is out of tune.
First, understand that high glucose levels can damage the endothelial lining, making vessels leaky and inviting fluid to pool in the lower extremities.
Second, nerve damage reduces the ability to feel the early swelling, so the condition can progress unnoticed.
Third, the kidneys, when overworked, lose their filtering finesse, leading to fluid retention that aggravates the edema.
Fourth, certain diabetes meds, especially thiazolidinediones, have a notorious side effect of water retention, so always discuss alternatives with your doctor.
Fifth, lifestyle plays a starring role – regular walks stimulate the calf muscle pump, encouraging venous return and shrinking that dreaded puffiness.
Sixth, keeping sodium low is non‑negotiable because excess salt shackles the kidneys into holding onto water.
Seventh, staying well‑hydrated paradoxically helps the body release excess fluid rather than hoarding it.
Eighth, compression stockings aren’t just a fashion statement; they apply graduated pressure that pushes fluid back toward the heart.
Ninth, elevating the legs above heart level for a few minutes each day can dramatically reduce swelling.
Tenth, diligent blood sugar monitoring reduces the cascade of vascular injury that fuels edema.
Eleventh, weight management lessens the pressure on veins and improves overall circulation.
Twelfth, routine skin checks prevent infections that can arise from stretched, compromised skin.
Thirteenth, if you notice pitting edema, seek medical advice promptly – it may herald deeper issues like heart or kidney disease.
Fourteenth, a balanced diet rich in potassium (think bananas and leafy greens) helps counteract sodium’s effects.
Fifteenth, never underestimate the power of a supportive healthcare team; they can tailor diuretics or other interventions to your unique needs.
In essence, edema in diabetes is a multi‑faceted challenge, but with proactive care, education, and a dash of perseverance, we can keep the swelling at bay and live a fuller, healthier life.
Tamara de Vries
May 14, 2023 AT 13:45hey yall, just a lil reminder that if ur meds are making u swell, talk 2 ur doc ASAP.
sometimes a simple switch can make a big diff and u wont feel like ur foot is a water balloon.
stay positive and keep movin, even a short walk helps!!
Jordan Schwartz
May 15, 2023 AT 04:11Empathy first: I’ve seen how edema can creep up on people with diabetes, and it’s easy to feel frustrated.
Take it one day at a time, focus on gentle exercise, and keep your doctor in the loop about any swelling changes.
Nitin Chauhan
May 15, 2023 AT 16:41Stay active keep sodium low elevate legs and stay on top of sugar levels
Angelo Truglio
May 16, 2023 AT 05:45Wow!!! This is absolutely the most *dramatic* overview I have ever read!!!
Who knew edema could be so *intricate*??!
Seriously, if you don’t follow these steps, you might as well be inviting a flood into your shoes!!!
Do *not* ignore the tiny warning signs – they’re screaming louder than a rock concert!!!
Dawn Midnight
May 16, 2023 AT 17:41While your enthusiasm is appreciated, the article contains several grammatical inaccuracies, such as the misuse of “its” versus “it’s.” Additionally, the phrasing could be more concise.
frank hofman
May 17, 2023 AT 06:28Actually, all that elevation stuff is just hype.
Dannii Willis
May 17, 2023 AT 18:41I find the information quite thorough and presented in a balanced manner. It’s nice to see the emphasis on both lifestyle and medical interventions.
Robyn Du Plooy
May 18, 2023 AT 06:05From a clinical perspective, the pathophysiology outlined aligns well with current vascular‑renal‑neuropathy models. However, incorporating more quantitative data on fluid shifts could enhance the evidence base.
Boyd Mardis
May 18, 2023 AT 18:01Concise tip: elevate, compress, hydrate.
ayan majumdar
May 19, 2023 AT 05:08good points but remember to keep checking blood pressure too
Johnpaul Chukwuebuka
May 19, 2023 AT 16:48Simple advice works best – drink water, move a little each day, and keep salt low.
Xavier Hernandez
May 20, 2023 AT 03:38We must hold ourselves accountable; ignoring fluid retention is a moral failure when we have the knowledge to act.
Zach Yeager
May 20, 2023 AT 14:11Honestly, the whole thing is overblown – most people will never see serious issues if they just eat right.
Angel Gallegos
May 21, 2023 AT 00:11While I appreciate the effort, the article feels overly simplistic, bordering on condescension. A deeper dive into the hemodynamic mechanisms would serve an educated audience better.
ANTHONY COOK
May 21, 2023 AT 09:55Let’s be real, the health industry loves to scare us into buying pricey meds – keep it simple, stay active, and watch the swelling melt away. 😏
Sarah Aderholdt
May 21, 2023 AT 19:21Philosophically, edema reminds us that the body seeks balance; when we disturb that equilibrium, it manifests visibly.
Phoebe Chico
May 22, 2023 AT 04:31Friends, let’s charge forward with vigor! Our bodies deserve the brightest, most vibrant care – no swelling shall hold us back!