Introduction to Carcinoma and Viral Infections
As a blogger passionate about health and wellness, I have always been intrigued by the connections between various diseases and their causes. One such connection that has caught my attention recently is the link between carcinoma and viral infections. Carcinoma, a type of cancer, has been found to have associations with certain viral infections, which can increase an individual's risk of developing cancer. In this article, I will discuss the various aspects of this connection, including the viruses involved, how they contribute to carcinoma development, and the preventive measures that can be taken to reduce the risk of infection and cancer.
Understanding Carcinoma: Definition and Types
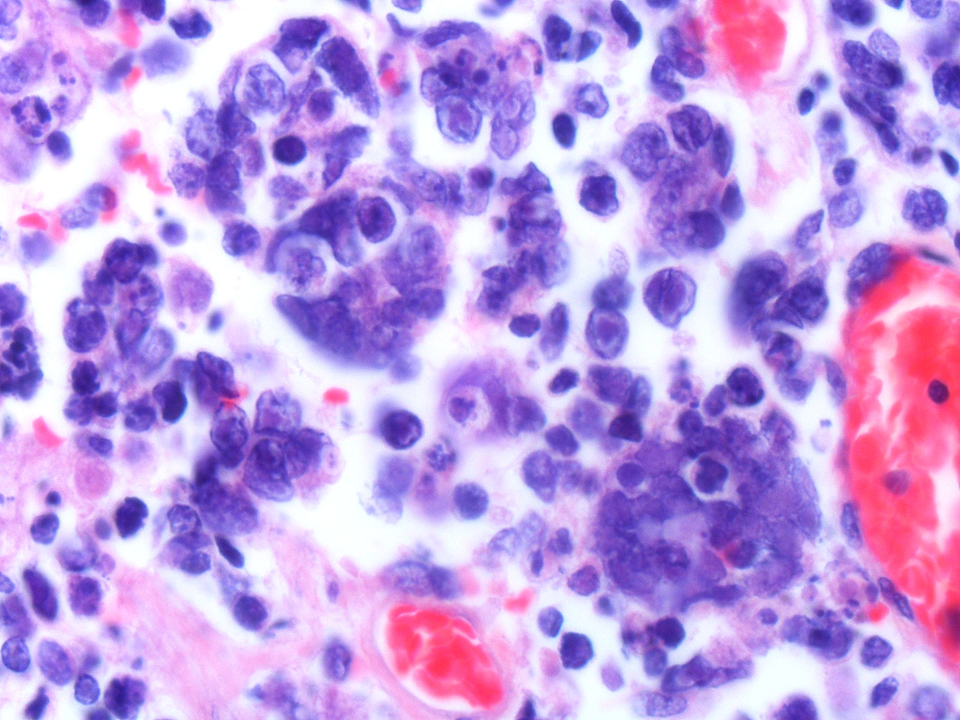
Before delving into the connection between carcinoma and viral infections, let us first understand what carcinoma is. Carcinoma is a type of cancer that originates in the epithelial cells, which are the cells that line the outer surfaces of our organs and tissues. There are several types of carcinomas, including basal cell carcinoma, squamous cell carcinoma, and adenocarcinoma, each affecting different types of epithelial cells. These cancers can occur in various parts of the body, such as the skin, lungs, breast, colon, and prostate.
Common Viruses Linked to Carcinoma Development
Several viruses have been identified to have a connection with the development of carcinoma. Some of the most common ones include:
1. Human Papillomavirus (HPV)
HPV is a group of more than 200 related viruses, some of which have been found to cause cervical, anal, and oropharyngeal cancers. High-risk types of HPV, such as HPV 16 and 18, are responsible for the majority of these carcinomas.
2. Hepatitis B and C Viruses (HBV and HCV)
Both HBV and HCV are known to cause liver cancer or hepatocellular carcinoma. Chronic infection with either of these viruses can lead to liver damage, cirrhosis, and eventually carcinoma.
3. Epstein-Barr Virus (EBV)
EBV is a member of the herpesvirus family and has been associated with the development of nasopharyngeal carcinoma and certain types of lymphomas.
4. Human T-cell Lymphotropic Virus Type 1 (HTLV-1)
HTLV-1 is a retrovirus that has been linked to adult T-cell leukemia/lymphoma, a type of non-Hodgkin lymphoma.
How Viral Infections Contribute to Carcinoma Development
Now that we have identified some of the common viruses linked to carcinoma, it is essential to understand how these viral infections contribute to cancer development. The mechanisms vary depending on the virus involved, but some common ways include:
1. Viral Oncogenes
Some viruses carry oncogenes, which are genes that have the potential to cause cancer. When these viruses infect a host cell, the viral oncogenes can interfere with the normal functioning of the cell, leading to uncontrolled growth and the formation of tumors.
2. Chronic Inflammation
Chronic viral infections can lead to ongoing inflammation in the infected tissue. This inflammation can cause damage to the cells and their DNA, increasing the risk of cancerous changes and tumor growth.
3. Immunosuppression
Some viruses, such as HIV, can weaken the immune system, making it harder for the body to fight against cancer cells and increasing the risk of developing carcinoma.
Preventing Viral Infections to Reduce Carcinoma Risk
Given the connection between viral infections and carcinoma, it is crucial to take preventive measures to reduce the risk of infection and, in turn, reduce the risk of cancer. Some of these preventive measures include:
1. Vaccination
Getting vaccinated against viruses like HPV and hepatitis B can help protect against these infections and their associated cancers. Talk to your healthcare provider about the appropriate vaccines for you and your family.
2. Safe Sex Practices
Using condoms and practicing safe sex can help reduce the risk of contracting sexually transmitted infections like HPV and HIV.
3. Regular Screening
Regular screening for cervical cancer through Pap tests and HPV tests can help detect precancerous changes early and prevent the development of cervical cancer.
4. Avoiding Risk Factors
Avoiding risk factors such as excessive alcohol consumption, smoking, and exposure to certain chemicals can help reduce the risk of liver cancer caused by hepatitis B and C infections.
Conclusion
In conclusion, the connection between carcinoma and viral infections is an essential aspect of understanding cancer development and prevention. By understanding the viruses involved, the mechanisms through which they contribute to carcinoma, and the preventive measures that can be taken, we can work towards reducing the risk of infection and cancer for ourselves and our loved ones. Stay informed, stay protected, and stay healthy.

5 Comments
Asia Lindsay
April 30, 2023 AT 04:50Great overview-stay safe, get vaccinated, and keep those check‑ups regular! 😊
Angela Marie Hessenius
April 30, 2023 AT 05:00Thank you for shedding light on such a critical intersection between oncology and virology; the depth of this topic truly warrants an extensive discussion.
From a global perspective, societies have long grappled with the dual burden of infection and cancer, often in ways that intertwine traditional practices with modern medicine.
In many East Asian cultures, for instance, regular health examinations are integrated into communal rituals, which has historically facilitated earlier detection of virally‑induced neoplasms.
Similarly, Scandinavian public‑health models emphasize widespread vaccination programs, reflecting a societal commitment to preventative care that transcends individual responsibility.
The historical lineage of the HPV vaccine, originally rooted in research collaborations across continents, exemplifies how scientific diplomacy can bridge cultural divides.
When we examine hepatitis B’s prevalence in sub‑Saharan Africa, we see that limited access to safe medical needles and cultural taboos surrounding bloodborne diseases exacerbate carcinogenic risk.
Conversely, in South America, community‑based education campaigns have successfully reduced the incidence of liver cancer by promoting safe injection practices and awareness of viral transmission.
These examples underscore that the fight against virus‑associated carcinomas is not merely a biomedical challenge but also a sociocultural one.
The mechanisms you described-viral oncogenes, chronic inflammation, and immunosuppression-are universal, yet their impact is modulated by local health infrastructure, dietary habits, and even religious beliefs about disease.
For example, certain dietary staples rich in antioxidants can mitigate oxidative stress caused by chronic inflammation, potentially lowering cancer risk.
Moreover, the stigma attached to sexually transmitted infections in many regions can discourage individuals from seeking HPV screening, thereby allowing precancerous lesions to progress unnoticed.
In light of this, culturally sensitive public‑health messaging becomes indispensable; it must respect local values while delivering evidence‑based recommendations.
Education initiatives that involve community leaders, healers, and teachers have proven effective in demystifying viral transmission pathways and encouraging vaccination uptake.
Furthermore, the integration of traditional healing practices with conventional medical protocols can foster trust, leading to higher compliance with screening schedules.
In summary, while the molecular biology of virus‑induced carcinogenesis is fascinating and complex, its translation into effective prevention strategies hinges on our ability to navigate diverse cultural landscapes with empathy and scientific rigor.
I appreciate your comprehensive overview and hope this dialogue encourages more cross‑disciplinary collaborations that honor both science and culture.
Julian Macintyre
April 30, 2023 AT 05:10While the article presents a thorough overview of oncogenic viruses, it omits a critical discussion of the epidemiological data supporting causality, such as relative risk ratios derived from cohort studies.
Furthermore, the mechanistic pathways described could be elaborated with references to the viral integration sites within the host genome, which are pivotal for malignant transformation.
It is also noteworthy that the role of co‑factors, including alcohol consumption and tobacco use, is downplayed despite their synergistic effects with hepatitis viruses.
The omission of these nuances may lead readers to underestimate the multifactorial nature of carcinoma development.
Nonetheless, the emphasis on vaccination aligns with current public‑health guidelines and should be commended.
Future revisions would benefit from incorporating a more rigorous appraisal of the primary literature to substantiate the claims made herein.
Patrick Hendrick
April 30, 2023 AT 05:20Awesome post!!! Stay informed; stay protected; stay healthy!!!
abhishek agarwal
April 30, 2023 AT 05:30Look, if you’re not getting the HPV and hepatitis B shots, you’re basically signing up for a fast track to cancer, period. No excuses, no drama-just get vaccinated and skip the future hospital bills.