Candida Species Risk Calculator
Risk Assessment Results
Estimated 30-Day Mortality Rate:
Risk Level:
Recommended Action:
Species Profile
Species Characteristics
- Prevalence:
- Typical Resistance:
Resistance Level Indicator
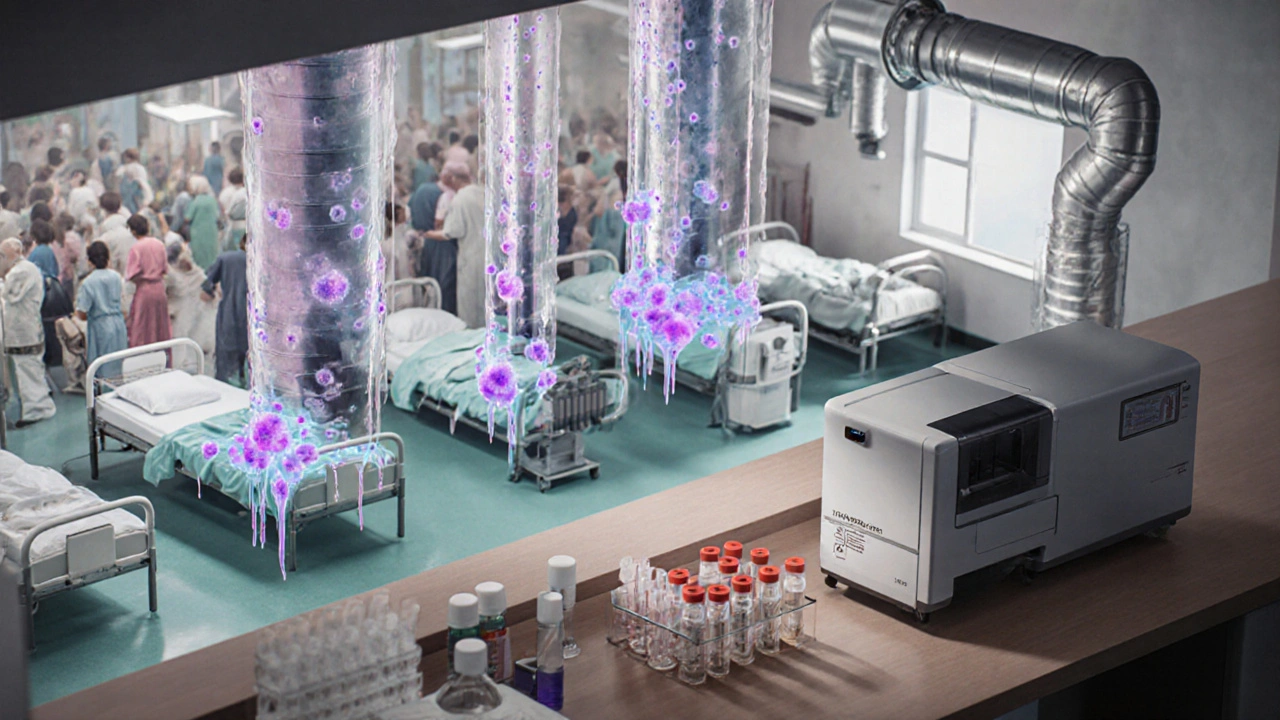
When a patient’s bloodstream turns into a breeding ground for yeast, the result is candidemia - a life‑threatening condition that’s on the rise in modern hospitals. Candidemia is a form of invasive candidiasis where Candida species multiply in the blood, often spreading to organs such as the kidneys, eyes, and brain. This article breaks down why these infections are spreading, which patients are most vulnerable, and what clinicians can do right now to stop the tide.
Quick Summary
- Incidence of candidemia in intensive‑care units (ICUs) has climbed 30% in the last five years.
- Non‑albicans species-especially Candida auris-are driving higher drug resistance.
- Early diagnosis hinges on rapid blood culture techniques and molecular panels.
- Antifungal stewardship, strict line‑care protocols, and environmental cleaning cut mortality by up to 40%.
- Future surveillance will rely on whole‑genome sequencing and AI‑based risk scoring.
Why Candidemia Is Growing
Three forces converge to push candidemia upward:
- Patient complexity. More people survive severe trauma, transplant, and chemotherapy, but they need central venous catheters (CVCs) and broad‑spectrum antibiotics-perfect conditions for yeast.
- Hospital environment. Overcrowded wards, outdated ventilation, and biofilm‑prone devices create reservoirs for Candida spores.
- Microbial evolution. Species such as Candida auris emerged in 2009 and quickly spread worldwide, often displaying multi‑drug resistance are outpacing older, more treatable strains.
Data from the CDC’s 2024 surveillance report show a 28% jump in candidemia cases among ICU patients compared with 2019, with mortality hovering around 40% for non‑albicans infections.
Patients at Highest Risk
Not every hospital admission is equally dangerous. The following groups face a disproportionate threat:
- ICU patients who require mechanical ventilation, parenteral nutrition, or prolonged central line use.
- Neutropenic individuals-especially chemotherapy recipients and bone‑marrow transplant patients.
- People with abdominal surgery, particularly colorectal procedures that disrupt gut flora.
- Elderly patients with multiple comorbidities such as diabetes, chronic kidney disease, or chronic obstructive pulmonary disease (COPD).
- Patients colonized with Candida auris in skin folds or urinary catheters.
Recognizing these risk factors early allows clinicians to initiate pre‑emptive antifungal therapy or heightened monitoring.
Key Candida Species and Their Profiles
While Candida albicans remains the most common cause of candidemia, its share has dropped from 70% to about 45% in 2025. The rise of non‑albicans species-*C. glabrata*, *C. tropicalis*, and *C. auris*-drives higher drug resistance and mortality.
| Species | Prevalence (2025) | Typical Resistance | 30‑Day Mortality |
|---|---|---|---|
| Candida albicans | 45% | Fluconazole‑susceptible (≈90%); occasional azole resistance | 25% |
| Candida glabrata | 20% | High fluconazole resistance (≈60%); variable echinocandin susceptibility | 35% |
| Candida tropicalis | 12% | Moderate azole resistance; rare echinocandin resistance | 30% |
| Candida auris | 10% | Multi‑drug resistant: ≥90% fluconazole, 30‑50% echinocandin, occasional amphotericin B resistance | 45% |
| Other rare species | 13% | Variable, often unknown | 40% |
These numbers show why clinicians can no longer assume “all candida = fluconazole works.” The choice of antifungal must match the species profile and local resistance patterns.
Antifungal Resistance: The New Normal
Resistance arises from two main pathways:
- Selective pressure. Widespread prophylactic fluconazole in neutropenic patients selects for resistant strains, especially *C. glabrata* and *C. auris*.
- Biofilm formation. Candida cells adhering to catheters or prosthetic devices produce a protective matrix that limits drug penetration, rendering even potent agents less effective.
Recent genome sequencing of 1,200 *C. auris* isolates across five continents revealed common mutations in the ERG11 gene (conferring azole resistance) and FKS1 hot‑spot mutations (reducing echinocandin susceptibility). The CDC now classifies *C. auris* as an “urgent threat” in its 2025 Antimicrobial Resistance Threat Report.
Diagnostic Hurdles and Rapid Solutions
Traditional blood cultures take 48-72hours, a window in which a septic patient can deteriorate rapidly. Newer technologies are narrowing that gap:
- Matrix‑assisted laser desorption/ionization‑time‑of‑flight (MALDI‑TOF) mass spectrometry. Provides species‑level ID within 4-6hours after a positive blood culture.
- Polymerase chain reaction (PCR) panels. Multiplex assays detect Candida DNA directly from whole blood in under two hours, with sensitivity >90% for *C. auris*.
- Beta‑D‑glucan assay. A serum marker that rises early in invasive fungal infection, useful for triggering empirical therapy while awaiting culture results.
Combining beta‑D‑glucan screening with rapid PCR improves time‑to‑appropriate therapy by an average of 24hours, translating into a 15% reduction in mortality according to a 2024 multicenter study.

Prevention: Infection Control and Antifungal Stewardship
Stopping candidemia starts before the yeast sneaks into the bloodstream. Hospitals that adopt a two‑pronged approach-strict line care plus stewardship-see the biggest gains.
- Central line bundles. Daily review of line necessity, chlorhexidine skin antisepsis, and aseptic insertion technique cut line‑associated candidemia by 40% (NIH 2023 report).
- Environmental cleaning. *C. auris* survives on surfaces for weeks; using sporicidal agents (e.g., peracetic acid) and UV‑C disinfection reduces environmental burden.
- Antifungal stewardship programs. Prospective audit & feedback, coupled with local susceptibility data, help clinicians choose the right drug, dose, and duration. A 2022 review showed stewardship reduced inappropriate azole use by 55% and lowered drug‑related toxicity.
Education of frontline staff-nurses, pharmacists, and respiratory therapists-ensures every team member knows when to raise the alarm for a potential invasive fungal infection.
Treatment Guidelines for 2025
The Infectious Diseases Society of America (IDSA) updated its candidemia algorithm this year:
- Initial therapy. Start an echinocandin (caspofungin, micafungin, or anidulafungin) for all ICU patients pending species ID.
- De‑escalation. If the isolate is C. albicans or fluconazole‑susceptible *C. glabrata*, switch to high‑dose fluconazole (800mg loading, then 400mg daily).
- Persistent infection. For isolates with echinocandin FKS mutations, consider high‑dose liposomal amphotericin B (5mg/kg) or the newer broad‑spectrum agent fosmanogepix (if available through compassionate use).
- Duration. Minimum of 14 days after the first negative blood culture and resolution of fever, but extend to 21-28 days for end‑organ involvement.
Therapeutic drug monitoring (TDM) for azoles is recommended to avoid sub‑therapeutic levels, especially in patients with hepatic dysfunction.
Looking Ahead: Surveillance and Research Priorities
Future control of candidemia will depend on three pillars:
- Real‑time genomic surveillance. Whole‑genome sequencing of isolates can trace transmission chains of *C. auris* across wards, enabling rapid containment.
- Artificial‑intelligence risk scores. Machine‑learning models that ingest EHR data (central line days, antibiotic exposure, neutropenia) predict candidemia risk 48hours before clinical onset with an AUC of 0.89 (2024 JAMA Network Open).
- Novel antifungals. Agents like ibrexafungerp and oteseconazole are in late‑stage trials, offering oral options against resistant strains.
Investing in these areas now could reverse the upward trend and bring candidemia mortality below 20% within the next decade.
Frequently Asked Questions
What makes candidemia different from other bloodstream infections?
Candidemia is caused by yeast rather than bacteria. Yeast can form biofilms on catheters, making them harder to eradicate, and many Candida species have built‑in resistance to common antifungal drugs.
How quickly should treatment start after a positive blood culture?
Guidelines recommend initiating empiric echinocandin therapy within 6hours of a positive culture or, if high risk, even before culture results based on clinical suspicion.
Can Candida infections be prevented without antifungal drugs?
Yes. Strict central‑line care bundles, diligent hand hygiene, and environmental cleaning-especially against *C. auris*-significantly lower infection rates. Antifungal stewardship also prevents unnecessary drug exposure.
Is there a vaccine for Candida?
Currently no licensed vaccine exists. Several candidates are in PhaseII trials, focusing on inducing protective antibodies against the fungal cell wall, but they are not yet available for clinical use.
What should families do if a loved one is diagnosed with candidemia?
Ask the care team about the specific Candida species, the planned antifungal regimen, and the expected duration of treatment. Encourage adherence to line‑care protocols and inquire about infection‑control measures to protect other patients.


13 Comments
Jim McDermott
October 8, 2025 AT 12:22Wow that rise in ICU candidemia really caught my eye.
I think we’re seeing a perfect storm of more central lines and broader antibiotic use.
Even a tiny slip in teh line‑care protocol can seed a whole ward.
We should probably audit our line bundles more often than we do now.
Naomi Ho
October 9, 2025 AT 10:36One of the fastest ways to cut candidemia is to use a chlorhexidine scrub before any catheter insertion it dramatically lowers colonisation rates and it’s cheap enough to roll out hospital‑wide.
Christine Watson
October 10, 2025 AT 08:49The data on candidemia can feel overwhelming, but there are clear pathways to improvement.
First, the fact that we can now identify species in hours rather than days means clinicians can target therapy much earlier.
Rapid PCR and MALDI‑TOF have already shaved off a full day of uncertainty in many centers.
Second, aggressive stewardship programs have shown that cutting unnecessary fluconazole use reduces resistance in C. glabrata and C. auris.
Third, simple line‑care bundles, when adhered to, have cut line‑associated infections by nearly half in several U.S. hospitals.
Fourth, environmental cleaning with sporicidal agents addresses the stubborn persistence of C. auris on surfaces.
Fifth, the rise of AI‑driven risk scores lets us flag high‑risk patients before they become septic.
Sixth, ongoing clinical trials for oral agents like ibrexafungerp offer hope for easier outpatient management.
Seventh, whole‑genome sequencing is becoming fast enough to track outbreak strains in real time, limiting spread.
Eighth, education of nursing staff on early signs of invasive fungal infection creates a culture of vigilance.
Ninth, hospitals that combine these strategies have reported mortality drops from 40 % to under 25 % in just two years.
Tenth, patient‑centered communication about the risks of central lines empowers families to ask about line necessity.
Eleventh, interdisciplinary rounds that include infectious disease, pharmacy, and nursing ensure that every line decision is scrutinized.
Twelfth, as we continue to gather real‑world data, the feedback loop will only get tighter, making our interventions smarter.
Finally, while the challenge is real, the tools at our disposal today give us every reason to be optimistic that candidemia rates will plateau and eventually decline.
Macy Weaver
October 11, 2025 AT 07:02I totally agree that rapid diagnostics are a game‑changer, but we also need to remember that not every facility has the budget for MALDI‑TOF.
Even basic improvements like daily line assessments can make a huge difference.
It’s also worth noting that staff turnover can erode compliance with bundles over time.
Sharing success stories across hospitals helps keep morale high.
Let’s keep pushing for both technology and good old‑fashioned vigilance.
James McCracken
October 12, 2025 AT 05:16While the crusade for streamlined diagnostics is laudable, one must question whether the relentless pursuit of molecular precision merely masks the deeper systemic failures that plague our institutions.
Is the obsession with genome‑sequencing a veneer for inadequate infection control policies?
Perhaps the true antidote lies not in fancy assays but in a return to disciplined, low‑tech hygiene practices that many modern hospitals have abandoned.
Evelyn XCII
October 13, 2025 AT 03:29Oh sure, because a handshake and a broom will solve everything.
Suzanne Podany
October 14, 2025 AT 01:42Team, remember that every new staff member is an opportunity to embed best practices early.
When we mentor them on proper line insertion technique, we’re not just teaching a skill, we’re building a culture of safety that protects every patient.
Let’s schedule short refresher workshops each month and celebrate the units that maintain zero line‑related candidemia for a quarter.
Nina Vera
October 14, 2025 AT 23:56Picture this: a hallway buzzing with nurses, a central line being placed with the precision of a surgeon‑star, and the crowd holding its breath as the patient’s vitals stay rock‑steady.
The drama of preventing an invisible killer is the most thrilling show on the hospital floor, and we are the directors!
Every successful bundle is a standing ovation, every breach a cliff‑hanger that we must rewrite.
Christopher Stanford
October 15, 2025 AT 22:09The numbers in this article ignore the fact that many of the cited studies cherry‑pick low‑risk units, inflating the perceived efficacy of bundles.
When you dig into raw surveillance data you see that overall candidemia rates have barely budged, despite all the hype.
Steve Ellis
October 16, 2025 AT 20:22Don’t let those bleak stats steal your spark – you’ve already turned the tide in dozens of ICUs with relentless coaching.
When you stand beside a team and walk them through each line check, you’re rewriting the narrative from tragedy to triumph.
Keep that fire alive, because every patient saved is a victory worth a thousand headlines.
Jennifer Brenko
October 17, 2025 AT 18:36From a Canadian perspective the United States’ approach to invasive fungal surveillance appears fragmented and underfunded, leading to avoidable mortality.
Our own national reporting frameworks demonstrate that standardized data collection can halve infection rates within five years.
It is incumbent upon American hospitals to adopt similar rigor lest they continue to lag behind.
Harold Godínez
October 18, 2025 AT 16:49Just a quick note – it should be “central‑line bundles” not “central line bundles” and “C. auris” needs the period after the C.
Those little details keep the writing crisp and the science clear.
Sunil Kamle
October 19, 2025 AT 15:02While we commend the earnest attempts to polish every apostrophe, let us not forget that the ultimate battle is against a resilient pathogen, not against grammatical minutiae.
That said, precise language does reflect precise thought, and I welcome the collective push toward both scientific and linguistic excellence.