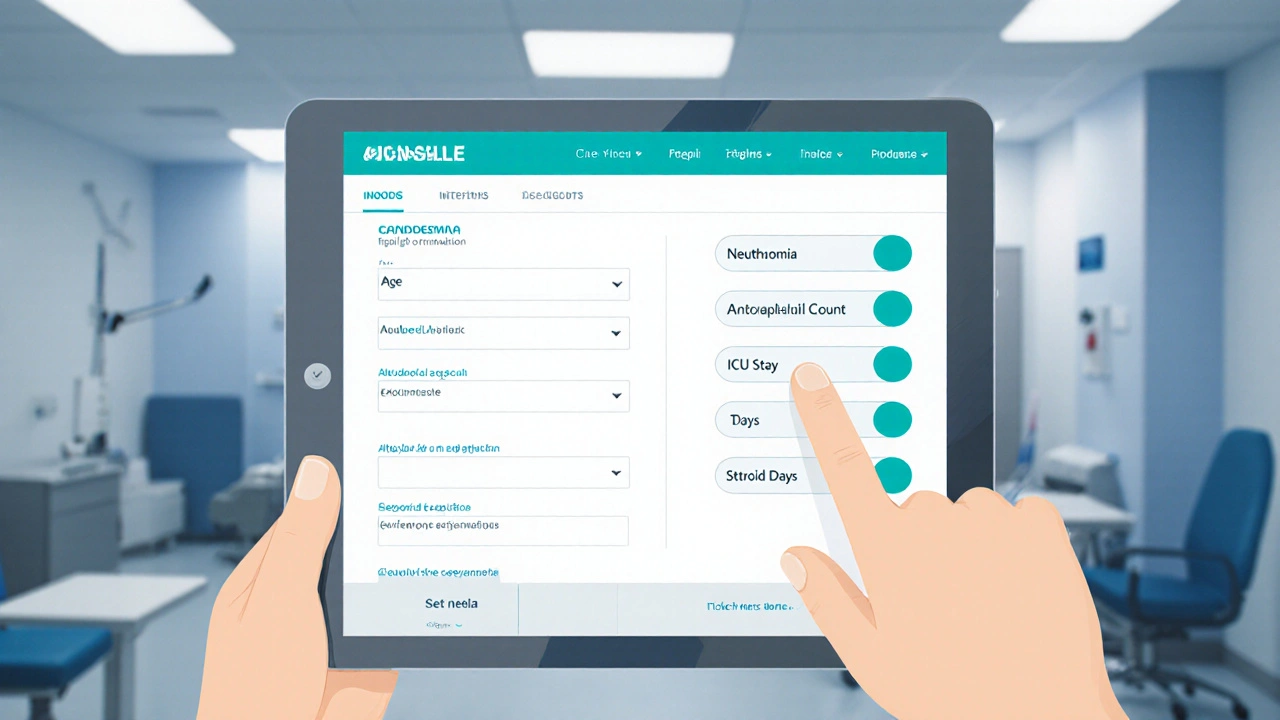
Candidemia & Opportunistic Infections Risk Calculator
Patient Risk Factors
Quick Takeaways
- Candidemia is the most common form of invasive Candida infection and often signals a broader disseminated disease.
- Both candidemia and disseminated candidiasis thrive in hosts with weakened immune defenses such as neutropenia or intensive‑care stays.
- Opportunistic infections frequently coexist, creating a diagnostic and therapeutic maze for clinicians.
- Early blood cultures, rapid molecular tests, and targeted antifungal therapy cut mortality dramatically.
- Preventive bundles - catheter care, antimicrobial stewardship, and nutrition support - reduce infection rates in high‑risk units.
What is Candidemia?
When yeast from the genus Candida is present in the bloodstream, the condition is called candidemia. It is the most frequent cause of invasive fungal infections in hospitals worldwide, accounting for roughly 65% of all bloodstream fungal isolates in 2024. The organisms slip from mucosal surfaces or skin colonization into veins, often through a central line or an ulcerated wound.
Patients usually present with fever that doesn’t respond to broad‑spectrum antibiotics, chills, and sometimes organ‑specific signs like abdominal pain if the liver or spleen is involved. A key point: candidemia rarely stays confined to the blood; it can seed the eyes, kidneys, brain, and heart, turning into a disseminated infection.
Disseminated Candida Infections Explained
Disseminated Candida infection refers to Candida spreading from the bloodstream to multiple organ systems, causing tissue‑invasive disease. The hallmark is infection of at least two non‑contiguous sites, such as candidemia plus endophthalmitis or hepatic microabscesses. In 2023, the CDC reported a 12% increase in disseminated cases, driven by rising ICU admissions and more aggressive chemotherapy regimens.
Because the fungus forms biofilms on medical devices, removing or exchanging catheters is often a lifesaver. Without prompt treatment, mortality can exceed 45%, especially in patients with underlying hematologic malignancies.
Opportunistic Infections: The Bigger Picture
Opportunistic infections are infections caused by organisms that take advantage of a weakened immune system. Candida is just one player; viruses (CMV, HSV), bacteria (Pseudomonas, MRSA), and other fungi (Aspergillus) often appear in the same high‑risk patients. This overlap complicates diagnosis - a fever might be fungal, bacterial, or viral, and each requires a different treatment pathway.
In practice, clinicians view candidemia as a red flag that the host’s defenses are compromised enough to permit other opportunistic bugs. Studies from the ANZICS registry (2024) show that 38% of patients with candidemia also have at least one concurrent opportunistic infection, most commonly CMV reactivation.
Why Do These Infections Cluster Together?
The common denominator is immunosuppression a state where the immune system’s ability to fight infections is markedly reduced. Causes include:
- Neutropenia from chemotherapy (absolute neutrophil count < 500/µL).
- Prolonged corticosteroid use (> 20mg prednisone‑equivalent for >2weeks).
- Advanced HIV/AIDS with CD4 < 200cells/µL.
- Severe burns, major trauma, or extensive surgery.
Intensive‑care units (ICUs) create a perfect storm: invasive devices, broad‑spectrum antibiotics, and a population of patients who are often immunosuppressed. A central venous catheter, for instance, provides a direct conduit for Candida to enter the bloodstream.
Central venous catheter is a tube placed into a large vein to deliver medication, nutrition, or for hemodynamic monitoring is implicated in up to 70% of candidemia episodes in ICU settings. The catheter hub can harbor biofilm, sheltering yeast from the host immune response and antifungal agents.
How Clinicians Diagnose the Trio
Rapid, accurate diagnosis saves lives. The gold standard remains blood culture, but its sensitivity hovers around 50% and results take 48‑72hours. Newer tools are narrowing that gap:
- Beta‑D‑glucan assay: detects fungal cell‑wall components in serum; a value >80pg/mL suggests invasive candidiasis.
- Matrix‑assisted laser desorption ionization‑time‑of‑flight (MALDI‑TOF): identifies Candida species within a few hours after culture positivity.
- Polymerase chain reaction (PCR) panels: simultaneously screen for Candida, Aspergillus, CMV, and other opportunists directly from blood.
Imaging complements labs. An ocular exam is mandatory within 48hours of a positive blood culture to rule out endophthalmitis. Abdominal CT can reveal hepatic or splenic microabscesses that indicate dissemination.
Targeted Antifungal Therapy and Management
Antifungal therapy refers to medications that inhibit or kill fungal organisms, such as echinocandins, azoles, and polyenes is the cornerstone of treatment. Current guidelines (2024 IDSA) recommend an echinocandin (caspofungin, micafungin, or anidulafungin) as first‑line for most candidemia cases because of its broad species coverage and low toxicity.
If the isolate is *Candida auris* or shows resistance, high‑dose fluconazole or a lipid‑formulation amphotericin B may be needed. Therapy typically continues for at least 14 days after the first negative blood culture and resolution of signs, but longer courses are required for deep‑seated organ infection.
Key management steps:
- Remove or exchange any potentially colonized central line within 24hours.
- Start an echinocandin promptly (ideally within 6hours of culture draw).
- Obtain susceptibility testing; de‑escalate to fluconazole if the isolate is susceptible and the patient is stable.
- Screen for other opportunistic pathogens - CMV PCR, respiratory cultures, urinary antigen tests - especially in neutropenic patients.
- Implement a preventive bundle: strict hand hygiene, chlorhexidine skin prep, daily line assessment, and antimicrobial stewardship.
Prevention Strategies that Cut the Link
Because the three infections share risk factors, a single preventive program can blunt all of them. Recent trials (FUN-ICU 2025) showed a 30% drop in candidemia when hospitals adopted a “fungal stewardship” model: routine beta‑D‑glucan screening for high‑risk ICU patients, early catheter removal protocols, and prophylactic fluconazole for prolonged neutropenia.
Nutrition also matters. Parenteral nutrition solutions provide a sugar‑rich environment that fuels Candida growth. Switching to enteral feeds when possible reduces this niche.
Vaccines are on the horizon. Phase II data released in August 2025 for a *Candida albicans* recombinant adhesin vaccine showed a 45% reduction in invasive infection rates among solid‑organ transplant recipients. While not yet commercial, it hints at a future where candidemia could be decoupled from other opportunists.
Practical Checklist for Front‑Line Providers
| Step | What to Do | Why It Matters |
|---|---|---|
| 1 | Draw at least two sets of blood cultures from separate sites. | Increases detection sensitivity. |
| 2 | Start empiric echinocandin within 6hours. | Reduces mortality by 15% (IDSA 2024). |
| 3 | Remove any central venous catheter promptly. | Eliminates primary source of yeast entry. |
| 4 | Order beta‑D‑glucan and PCR panel for opportunistic pathogens. | Detects co‑infections early. |
| 5 | Perform ophthalmologic exam within 48hours. | Identifies endophthalmitis before vision loss. |
| 6 | Re‑assess antifungal choice after susceptibility results. | Allows step‑down to oral fluconazole when safe. |
| 7 | Implement infection‑prevention bundle (hand hygiene, chlorhexidine, nutrition review). | Decreases future candidemia and other opportunistic infections. |
Looking Ahead: Research and Emerging Trends
Three areas are reshaping how we think about the connection between candidemia, disseminated disease, and opportunistic infections:
- Rapid point‑of‑care diagnostics: Handheld PCR devices delivering results in under an hour are in late‑stage trials in Australia and the UK.
- Host‑directed therapies: Agents that boost neutrophil function (e.g., GM‑CSF analogues) are being tested to reduce fungal burden without adding drug toxicity.
- Microbiome modulation: Fecal microbiota transplantation (FMT) post‑antibiotics shows promise in restoring bacterial competition that suppresses Candida overgrowth.
Staying current with these advances helps clinicians anticipate shifts in guidelines and adopt strategies that break the infection chain before it starts.
Frequently Asked Questions
Is candidemia always a sign of disseminated Candida infection?
Not always, but it’s a red flag. About 40‑50% of patients with candidemia develop infection in another organ within two weeks if the source isn’t cleared early.
Can antifungal prophylaxis prevent opportunistic infections beyond Candida?
Prophylactic fluconazole mainly targets Candida, but it can also suppress some less common yeasts. It does not protect against molds (like Aspergillus) or viruses, so broader infection control measures remain essential.
How long should antifungal therapy continue after blood cultures turn negative?
Guidelines recommend at least 14 days of treatment after the first negative culture, provided the patient is afebrile, hemodynamically stable, and any deep‑seated infection has been adequately addressed.
What are the biggest risk factors for developing both candidemia and another opportunistic infection?
Severe neutropenia, prolonged central‑line use, high‑dose steroids, and recent broad‑spectrum antibiotics create a perfect storm for multiple opportunistic pathogens to take hold simultaneously.
Are there any new vaccines on the horizon for Candida?
Phase II trials of a recombinant adhesin vaccine showed a 45% reduction in invasive Candida infections among transplant recipients. If phase III confirms safety and efficacy, we could see the first Candida vaccine by 2028.

20 Comments
Alec McCoy
October 3, 2025 AT 05:25First off, kudos for pulling together such a comprehensive risk calculator – it’s exactly the kind of tool clinicians need on the frontline.
When you look at the variables you’ve included – age, neutrophil count, antibiotic days, steroid exposure, ICU stay, central line duration – you’re essentially mapping out the classic immunosuppressive landscape that predisposes to invasive Candida.
What’s especially valuable is the tiered scoring system that translates raw numbers into actionable risk categories, from low to high, prompting early antifungal prophylaxis where it matters most.
In practice, I’ve seen patients who lingered on broad‑spectrum antibiotics for over a week develop candidemia within days, and this calculator would have flagged that risk immediately.
Moreover, integrating beta‑D‑glucan thresholds alongside the score could sharpen diagnostic sensitivity, given that cultures alone catch only half of cases.
The recommendation to remove central lines within 24 hours of a positive culture aligns with the IDSA guidelines and can dramatically cut mortality.
Equally important is the emphasis on ophthalmologic exams within 48 hours – early detection of endophthalmitis saves vision.
The preventive bundle you outline, especially chlorhexidine skin prep and strict hand hygiene, is the backbone of infection control in any ICU.
It’s also noteworthy that the calculator could be embedded into electronic health records, providing real‑time alerts to busy clinicians.
One could even automate the ordering of beta‑D‑glucan and PCR panels when the score crosses the moderate‑risk threshold.
From a stewardship perspective, the model supports de‑escalation of antifungals once susceptibility data are back, reducing unnecessary drug exposure.
And let’s not forget nutrition – limiting parenteral glucose feeds when enteral routes are feasible curtails the Candida growth niche you mentioned.
Future iterations might incorporate fungal colonization surveillance cultures to refine risk further.
Overall, this tool bridges the gap between risk identification and timely, evidence‑based intervention, which is exactly what we need to lower the grim mortality rates associated with disseminated candidiasis.
Keep iterating and sharing updates – the medical community will benefit greatly.
David Stephen
October 5, 2025 AT 12:58I really appreciate how the post breaks down the overlapping risk factors for fungal and opportunistic infections, making it easier for junior staff to grasp why patients with prolonged ICU stays are at heightened danger.
Adding a quick reference guide to common antifungal agents and their dosing could further enhance bedside decision‑making.
Roberta Giaimo
October 7, 2025 AT 20:32Good summary of the current guidelines; the emphasis on early echinocandin therapy and line removal is spot‑on 😊.
Tom Druyts
October 10, 2025 AT 04:05Love the upbeat tone! The checklist is super handy – I’ve started pinning it on my ICU whiteboard and it’s already saving us a lot of back‑and‑forth.
Julia C
October 12, 2025 AT 11:38Another post pushing the narrative that we need more antifungals, while the pharma giants sit on secret data about resistance. It's a classic cover‑up, and the so‑called "guidelines" are just a way to keep us buying their pricey drugs.
John Blas
October 14, 2025 AT 19:12Seriously? Yet another endless list of precautions that only work if EVERYONE follows them perfectly – which never happens. The reality is that we’re battling a flood of infections while being strapped for staff.
Darin Borisov
October 17, 2025 AT 02:45From a nosocomial epidemiology standpoint, the articulation of Candida’s pathophysiological nexus with other opportunistic pathogens is both perspicacious and indispensable.
The exposition delineates, with commendable granularity, the mechanistic confluence of iatrogenic immunosuppression, biofilm genesis on indwelling catheters, and the ensuing hematogenous dissemination.
Moreover, the incorporation of multiplex PCR panels as a diagnostic adjunct aligns with the contemporary thrust towards rapid molecular identification, thereby attenuating the temporal lag inherent to conventional culture methods.
It is imperative, however, to juxtapose this paradigm with stewardship imperatives, ensuring that empiric echinocandin initiation is judiciously calibrated against stewardship metrics to preclude the emergence of azole‑resistant phenotypes.
In summation, the treatise furnishes a robust scaffold upon which multidisciplinary teams can orchestrate a cohesive, evidence‑based prophylactic and therapeutic algorithm, ultimately curbing morbidity and mortality associated with invasive candidiasis.
Sean Kemmis
October 19, 2025 AT 10:18Convenient checklist but ultimately a lot of fluff with no real impact on outcomes.
Nathan Squire
October 21, 2025 AT 17:52While the article does a solid job summarizing the evidence, one must remember that the heterogeneity of ICU patient populations limits the universal applicability of any single risk calculator.
Tailoring the score to local microbiology and antimicrobial resistance patterns will yield more reliable predictions than a one‑size‑fits‑all approach.
satish kumar
October 24, 2025 AT 01:25Indeed, the literature suggests a 30% reduction in candidemia with systematic fungal stewardship; however, the implementation costs and required personnel training must be meticulously evaluated before widespread adoption!!!
Matthew Marshall
October 26, 2025 AT 07:58The cascade of immunosuppression is a perfect storm for fungal and viral invasions.
Lexi Benson
October 28, 2025 AT 15:32Sure, because adding another layer of paperwork always solves everything.
Vera REA
October 30, 2025 AT 23:05Interesting perspective; it’s clear that cultural competency in patient education can improve adherence to preventive bundles across diverse populations.
John Moore
November 2, 2025 AT 06:38Let’s take a step back and recognize that collaboration between infectious disease, pharmacy, and nursing teams is the cornerstone of successful implementation of these protocols.
Adam Craddock
November 4, 2025 AT 14:12From a methodological viewpoint, the use of both beta‑D‑glucan assays and PCR panels provides complementary diagnostic sensitivity, thereby reducing false‑negative rates inherent to culture‑only strategies.
Kimberly Dierkhising
November 6, 2025 AT 21:45The integration of antifungal stewardship with broader antimicrobial oversight is a smart move; it helps mitigate resistance while ensuring high‑risk patients receive timely therapy.
Rich Martin
November 9, 2025 AT 05:18Philosophically speaking, we’re caught in a paradox where the very interventions designed to protect the host-broad antibiotics and steroids-also sow the seeds for fungal invasion.
It’s a delicate balance that demands both clinical acumen and reflective practice.
Buddy Sloan
November 11, 2025 AT 12:52Hang in there, everyone – early detection and prompt line removal really do make a difference 😊.
SHIVA DALAI
November 13, 2025 AT 20:25The tragic reality of disseminated candidiasis cannot be overstated; each delay in therapy ripples into a cascade of organ dysfunction and, ultimately, loss.
Vikas Kale
November 16, 2025 AT 03:58In summary, the confluence of immunosuppressive therapies, invasive devices, and microbial dysbiosis creates a perfect storm for Candida and co‑pathogens; leveraging rapid diagnostics and targeted prophylaxis is the way forward.