Understanding Livedoid Vasculopathy and Betamethasone
Livedoid vasculopathy is a rare and chronic skin condition characterized by painful ulcers and lesions on the lower legs. It can greatly impact a patient's quality of life, making it crucial to explore effective treatment options. One potential treatment is betamethasone, a corticosteroid that has shown promise in alleviating the symptoms of livedoid vasculopathy. In this article, we will delve into the potential benefits of betamethasone for treating this condition and discuss the various aspects of this treatment approach.
Reducing Inflammation and Pain with Betamethasone
One of the primary benefits of betamethasone is its ability to reduce inflammation and pain associated with livedoid vasculopathy. As a corticosteroid, betamethasone works by suppressing the immune system's response, thereby reducing inflammation in the affected area. This can lead to a significant decrease in pain and discomfort experienced by patients, allowing them to engage in daily activities with greater ease. Additionally, the reduced inflammation can promote the healing of ulcers and prevent the formation of new ones.
Improving Skin Appearance and Healing
Another advantage of using betamethasone for livedoid vasculopathy is its ability to improve the appearance of the skin. The medication can help reduce redness, swelling, and the formation of scars, giving the skin a healthier and more even appearance. Furthermore, betamethasone can promote the healing process by encouraging the growth of new, healthy skin cells to replace damaged ones. This can result in faster recovery from ulcers and a reduced likelihood of recurrence.
Boosting Overall Quality of Life
By effectively managing the symptoms of livedoid vasculopathy, betamethasone can greatly improve a patient's overall quality of life. The reduction in pain and inflammation can lead to increased mobility and comfort, allowing patients to participate in daily activities without being held back by their condition. Additionally, the improved skin appearance can boost self-esteem and confidence, leading to better mental health and emotional well-being.
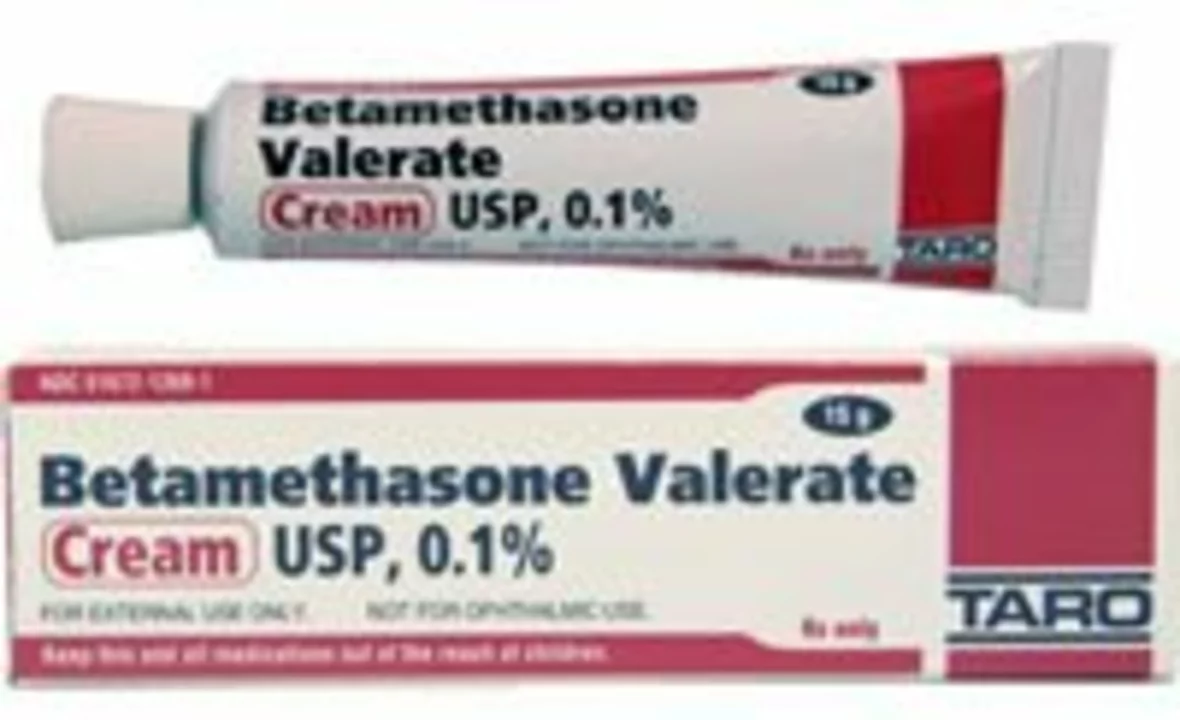
Convenient and Flexible Treatment Options
Betamethasone is available in various forms, such as creams, ointments, and injections, providing patients with flexible treatment options. This allows patients and healthcare providers to choose the most suitable form of treatment based on individual preferences and needs. Furthermore, the convenience of applying a cream or ointment at home can help patients maintain a consistent treatment routine, increasing the likelihood of successful symptom management.
Combining Betamethasone with Other Treatments
For some patients, betamethasone may be most effective when used in conjunction with other treatment approaches. This can include compression therapy, which helps improve blood flow in the affected area, or medications such as anticoagulants or immunosuppressants to address the underlying cause of the condition. Combining these treatments can provide a comprehensive approach to managing livedoid vasculopathy and ensuring the best possible outcome for patients.
Minimal Side Effects and Complications
Compared to other treatment options, betamethasone is generally well-tolerated and has a low risk of side effects and complications. Some potential side effects may include skin thinning or irritation, but these are typically mild and manageable. By following the prescribed treatment plan and monitoring for any adverse reactions, patients can safely benefit from the potential advantages of betamethasone for livedoid vasculopathy.
Discussing Betamethasone with Your Healthcare Provider
Given the potential benefits of betamethasone for treating livedoid vasculopathy, it is essential to have an open and honest discussion with your healthcare provider about this treatment option. They can help you determine if betamethasone is the right choice for your specific case and guide you through the appropriate dosage and application process. Remember, always follow your healthcare provider's recommendations and report any side effects or concerns that may arise during treatment.

17 Comments
Elijah Mbachu
May 19, 2023 AT 21:35I've seen a few patients with livedoid vasculopathy who responded well to a short course of betamethasone; the key is to start low and monitor the skin closely, making sure you dont overdo the steroid - a gentle approach usually keeps the inflammation in check while minimizing side effects.
Sunil Rawat
May 26, 2023 AT 09:26That sounds like a solid plan bhai, using a low potency cream first can really help the skin heal without causing too much thinning, and you can always step up if needed.
Andrew Buchanan
June 1, 2023 AT 21:16When prescribing betamethasone, it is essential to define the treatment duration and potency to avoid adverse effects such as atrophy, and to schedule follow‑up appointments for objective assessment of lesion improvement.
Krishna Chaitanya
June 8, 2023 AT 09:06Wow the skin can actually bounce back like magic when the steroid gets to work it’s like a storm clearing the sky and the pain just fades away
diana tutaan
June 14, 2023 AT 20:56While betamethasone does lower inflammation its long‑term use can lead to skin thinning and systemic effects that are often overlooked in short articles
Sarah Posh
June 21, 2023 AT 08:46It’s great that you’re looking at a balanced regimen; pairing the cream with proper compression can boost circulation and help sustain the healing gains.
James Knight
June 27, 2023 AT 20:36Honestly this steroid hype is just another pharma gimmick that promises miracles but leaves you with fragile skin and more pills to swallow.
Ajay D.j
July 4, 2023 AT 08:26Stay positive and keep tracking the response; even small improvements in ulcer size can make a big difference in daily comfort.
Dion Campbell
July 10, 2023 AT 20:16One must appreciate the nuanced interplay of corticosteroid pharmacodynamics and vascular pathology, yet the current discourse often reduces this to a superficial bullet‑point list that barely scratches the surface of clinical complexity.
Burl Henderson
July 17, 2023 AT 08:06From a therapeutic standpoint, integrating betamethasone into a multimodal protocol aligns with evidence‑based practice, especially when you consider the synergistic effect with anticoagulant therapy and compression garments.
Leigh Ann Jones
July 23, 2023 AT 19:56Betamethasone, as a potent glucocorticoid, offers a multifaceted approach to managing livedoid vasculopathy, beginning with its well‑documented anti‑inflammatory properties that directly target the cytokine cascade responsible for vascular damage. By attenuating the inflammatory response, the medication helps to reduce the edema and erythema that commonly accompany chronic ulceration. Moreover, the steroid’s ability to modulate immune cell infiltration can lead to a more organized and rapid re‑epithelialization process, which is critical for restoring the integrity of the skin barrier. Patients often report a noticeable decrease in pain within days of initiating therapy, which can translate to improved mobility and a higher quality of life. In addition to symptom relief, the reduction in inflammatory mediators may also prevent the formation of new ulcerative lesions, thereby curbing disease progression. The topical formulation provides a convenient delivery system, allowing for precise dosing and minimal systemic absorption, which is particularly advantageous for individuals with comorbidities. However, clinicians must remain vigilant for potential adverse effects, such as skin atrophy, telangiectasia, or hypothalamic‑pituitary‑adrenal axis suppression, especially with prolonged use. Regular follow‑up appointments enable the healthcare provider to assess the therapeutic response and adjust the regimen as needed. Combining betamethasone with compression therapy can further enhance venous return, thereby supporting the overall healing environment. Additionally, adjunctive anticoagulant therapy may address underlying hypercoagulable states that contribute to the pathogenesis of livedoid vasculopathy. Patient education plays a pivotal role; individuals should be instructed on proper application techniques to maximize efficacy and minimize irritation. Lifestyle modifications, including smoking cessation and weight management, can synergistically improve outcomes when paired with pharmacologic treatment. It is also beneficial to monitor laboratory parameters periodically to detect any systemic effects early. Ultimately, a personalized treatment plan that incorporates betamethasone alongside supportive measures offers the greatest chance for sustained remission. Continued research and clinical trials will further elucidate the optimal dosing strategies and long‑term safety profile of this therapeutic option.
Sarah Hoppes
July 30, 2023 AT 07:46They don’t want you to know the real side effects hidden in the fine print.
Robert Brown
August 5, 2023 AT 19:36Betamethasone is just a cheap band‑aid for lazy doctors.
Erin Smith
August 12, 2023 AT 07:26Don’t let the fear hold you back you’ve got the right tools to fight this.
George Kent
August 18, 2023 AT 19:16It’s absolutely essential that we, as responsible citizens of the United States, demand the highest‑quality evidence for any medication-especially a potent corticosteroid like betamethasone-before it reaches our patients! 🇺🇸💊
Jonathan Martens
August 25, 2023 AT 07:06Sure, because adding another steroid to the mix always solves everything.
Jessica Davies
August 31, 2023 AT 18:56Actually, the whole premise that betamethasone benefits livedoid vasculopathy is flawed; the literature is riddled with bias and the supposed “improvements” are nothing more than placebo effects.