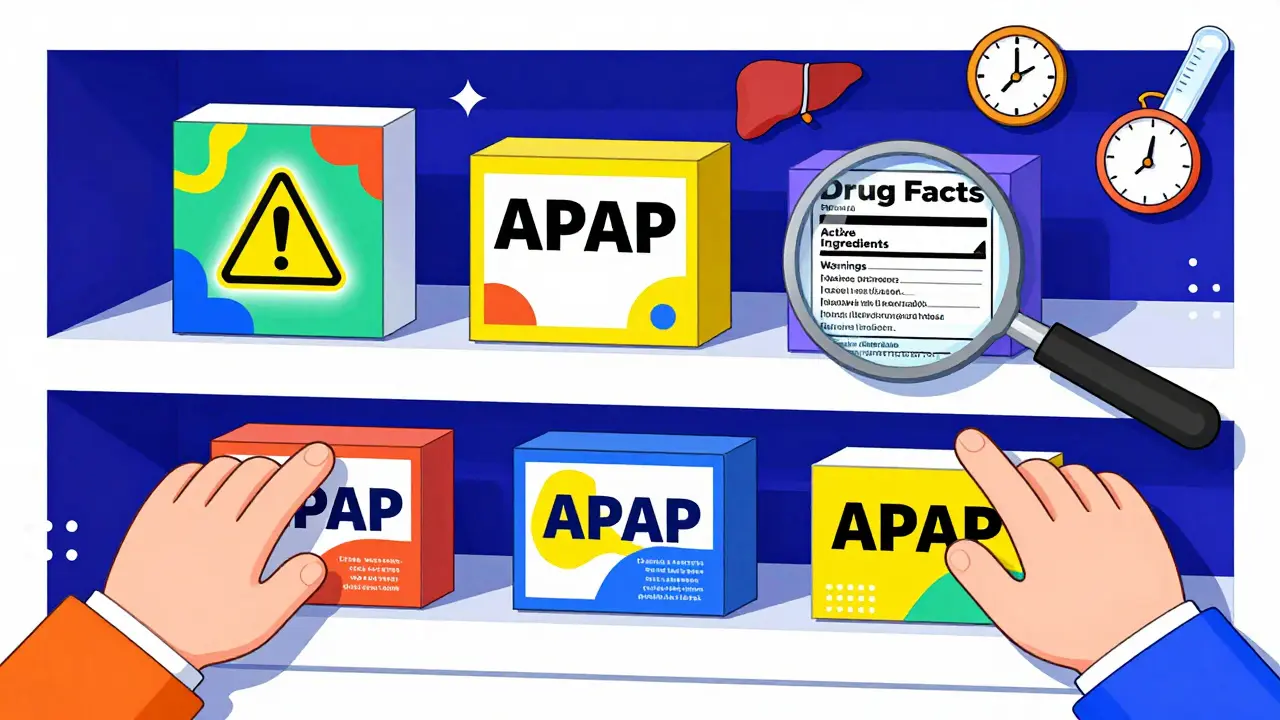
Read the Drug Facts label - every time
You wouldn’t buy a car without checking the manual, so why pick up a medicine without reading the label? The Drug Facts label isn’t just a formality - it’s your safety guide. Since 1999, the FDA has required every OTC medicine in the U.S. to use this standard format. It’s broken down into clear sections: active ingredients, purpose, uses, warnings, directions, and other information. The active ingredients section tells you exactly what’s in the pill or liquid. If you’re taking two different products, you might accidentally double up on the same ingredient - like acetaminophen. That’s how liver damage happens. One study found that nearly 20% of people who ended up in the ER for OTC overdose didn’t realize they were taking acetaminophen in more than one product. Always check this section. If you see the same ingredient on two boxes, don’t take both.
Know what’s in your medicine - especially acetaminophen
Acetaminophen is in more than 600 OTC products. It’s in Tylenol, but also in cold medicines, sleep aids, and even some prescription painkillers. The FDA says taking more than 4,000 milligrams in a day can cause serious liver damage. For some people - especially those who drink alcohol regularly, have liver disease, or are older - even 3,000 mg can be risky. The CDC reports that acetaminophen overdose leads to about 56,000 emergency room visits every year in the U.S. That’s not a small number. If you’re not sure whether your medicine has it, look for the word “acetaminophen” or the abbreviation “APAP” on the label. If you’re unsure, ask the pharmacist. They see this mistake every day.
Don’t guess the dose - measure it
“A spoonful” isn’t a real measurement. Kitchen spoons vary wildly in size. The FDA tested household spoons and found they could hold anywhere from 2 to 20 milliliters - that’s a 200% difference. Giving a child a “spoonful” of cough syrup could mean giving them double or triple the right dose. Always use the measuring tool that comes with the medicine - a dosing cup, syringe, or oral dropper. Never use a kitchen spoon. And never guess a child’s dose based on their size. The label gives dosing by age or weight. If your child is under two, or weighs less than 24 pounds, talk to a pharmacist before giving anything. The same goes for older adults. Metabolism slows with age, and what was safe at 40 might be too much at 70.
Choose single-ingredient medicines when you can
Multi-symptom cold and flu pills might seem efficient, but they’re often dangerous. If you only have a headache and a stuffy nose, you don’t need a product that also includes a cough suppressant, an antihistamine, and a decongestant. Each extra ingredient adds risk. For example, decongestants like pseudoephedrine can raise blood pressure - bad news if you have heart disease. Antihistamines like diphenhydramine can make you dizzy or cause urinary retention in men with enlarged prostates. The Ohio Department of Aging recommends picking medicines that treat only the symptoms you have. If you’re unsure, ask the pharmacist to help you pick a targeted option. You’ll get relief faster and avoid side effects you don’t need.

Talk to the pharmacist - it’s free
Pharmacists aren’t just the people who hand you your pills. They’re trained to spot dangerous combinations, flag interactions, and recommend the safest option for your health history. If you’re on blood pressure meds, diabetes drugs, or blood thinners, a simple OTC pain reliever could interfere. Aspirin and ibuprofen can thin your blood - risky if you’re on warfarin. Antihistamines can make sedatives stronger. Even herbal supplements like St. John’s wort can clash with OTC medicines. A 2022 study showed pharmacist consultations reduced medication errors by 67% in community pharmacies. You don’t need an appointment. Just walk up to the counter with your medicine in hand and ask: “Is this safe with what I’m already taking?” Most pharmacies offer this service at no cost. It takes two minutes. It could save your life.
Know when to skip OTC and see a doctor
OTC meds are great for headaches, mild colds, heartburn, or aching muscles. But they’re not for everything. If your symptoms last more than a few days, get worse, or come with fever, rash, or trouble breathing, don’t keep self-treating. People with chronic conditions - diabetes, kidney disease, heart failure, asthma - should always check with a doctor before using OTC products. Decongestants can spike blood sugar. Antacids with sodium can worsen heart failure. Some cold medicines contain alcohol or sugar, which can be harmful for diabetics. The Merck Manual says older adults, pregnant women, and young children are especially vulnerable to OTC risks. If you’re unsure whether your symptom is “minor” enough for OTC, err on the side of caution. A quick call to your doctor beats a trip to the ER.
Keep a medicine list - and update it
Most people don’t realize how many medications they’re taking. You might be on a prescription for high blood pressure, take a daily vitamin, use a topical cream for eczema, and grab a painkiller for your back. All of it matters. Keep a written or digital list of everything you take - including OTCs, supplements, and herbal products. Update it every time you start or stop something. Bring this list to every doctor visit and every pharmacy trip. It helps your pharmacist spot interactions you might miss. For example, if you’re taking melatonin for sleep and also use a cold medicine with diphenhydramine, you’re doubling up on sedatives. That’s not obvious unless someone sees the full picture.

Store medicines safely - and check expiration dates
Heat, moisture, and light can break down medicines. Don’t keep them in the bathroom cabinet - the steam ruins them. Store them in a cool, dry place, like a bedroom drawer. Keep them out of reach of kids and pets. And never take expired medicine. The FDA says expiration dates are the last day the manufacturer guarantees full potency and safety. After that, the medicine might not work - or it could break down into harmful substances. If you’re unsure whether a pill is still good, throw it out. Most pharmacies have take-back programs for expired or unused meds. Don’t flush them or toss them in the trash. Ask your pharmacist how to dispose of them safely.
Watch for red flags on the label
Not all OTC products follow the rules. Some herbal or “natural” supplements aren’t regulated the same way. They might not have a Drug Facts label at all. If you see claims like “cures arthritis” or “100% natural and safe,” be skeptical. The FDA doesn’t approve these products the same way it does OTC drugs. Look for the “Drug Facts” heading. If it’s missing, the product may not have been tested for safety or effectiveness. Also, avoid products with no manufacturer name, no lot number, or no expiration date. These are often sold online or in unregulated stores. Stick to brands you recognize from reputable pharmacies.
Use the same pharmacy every time
When you fill all your prescriptions and buy your OTC meds at the same pharmacy, the pharmacist builds a complete record of what you’re taking. That way, they can catch a dangerous interaction before you even leave the store. If you switch pharmacies, that history gets lost. One person might be taking three different painkillers from three different stores, and none of the pharmacists know about the others. That’s how accidental overdoses happen. Even if you only buy OTCs there, stick with one pharmacy. It’s one of the simplest, most effective safety steps you can take.
Be extra careful if you’re over 65
Older adults make up just 13% of the population but account for half of all adverse drug reactions from OTC meds. Why? Because metabolism slows down, kidneys don’t filter as well, and people often take multiple medications. A common cold pill with diphenhydramine might cause confusion or falls. A decongestant could raise blood pressure dangerously. The Merck Manual says seniors should avoid antihistamines, decongestants, and NSAIDs like ibuprofen unless approved by a doctor. Instead, try acetaminophen for pain (within safe limits), saline sprays for congestion, and warm compresses for sinus pressure. Always ask your pharmacist: “Is this safe for someone my age?”

13 Comments
Joie Cregin
January 15, 2026 AT 13:08I used to just grab whatever looked good until my grandma nearly went to the ER from mixing Tylenol and a cold med. Now I read every label like it’s a novel. Seriously, if you’re not checking for APAP, you’re playing Russian roulette with your liver. 🤯
Melodie Lesesne
January 15, 2026 AT 16:31This is so true. I started keeping a little note on my phone with everything I take-even the gummies. My pharmacist actually thanked me last time I went in. Small habit, huge difference.
Corey Sawchuk
January 16, 2026 AT 16:09Pharmacists are underrated heroes. I used to think they just handed out pills. Turns out they’re the only ones who actually know what’s in all those bottles. Just asked one yesterday about mixing melatonin with my sleep aid. Saved me from a bad night.
Stephen Tulloch
January 18, 2026 AT 02:34LMAO people still use kitchen spoons?? 😂 Bro you’re not cooking pasta, it’s medicine. If you can’t measure 5mL, maybe don’t self-medicate. Also why are you taking 4 different cold meds at once? You’re not a buffet.
Henry Ip
January 18, 2026 AT 20:57Biggest tip I’ve learned: if you’re not sure, don’t take it. Better to sit it out than end up in the ER because you thought 'it’s just one more pill.' I’ve stopped taking anything without checking the active ingredients first. Game changer.
Kasey Summerer
January 19, 2026 AT 23:53Oh so now we’re supposed to treat OTC meds like they’re nuclear codes? 🤡 I took NyQuil with Advil for 12 years and I’m still standing. Maybe your body’s just stronger than the fear-mongering labels.
Cheryl Griffith
January 21, 2026 AT 06:07My mom’s 72 and she refuses to ask pharmacists anything because she thinks they’ll judge her. But she takes 8 different things and still uses a teaspoon for cough syrup. I showed her this post and she finally agreed to let me go with her next time. It’s not about being scared-it’s about being smart.
Corey Chrisinger
January 22, 2026 AT 18:31It’s funny how we trust algorithms to pick our dating matches but won’t trust a label that’s been standardized for 25 years. We live in a world where we’ll research a $200 blender for 3 hours but grab a pill because the bottle looks pretty. There’s a deeper cultural issue here about responsibility and attention. We’ve outsourced care.
Bianca Leonhardt
January 24, 2026 AT 11:20If you don’t read labels, you deserve what you get. I’ve seen people take 3 different cold meds and then wonder why they’re dizzy, nauseous, and hallucinating. It’s not rocket science. It’s basic reading comprehension. Maybe try not being lazy?
Travis Craw
January 24, 2026 AT 18:21i used to think the pharmacist was just there to count pills but then i asked if my painkiller was okay with my blood pressure med and they literally stopped everything to explain it. like… they care. i feel kinda dumb now for not asking sooner
Christina Bilotti
January 25, 2026 AT 10:30Oh wow, you mean the FDA actually has standards? Who knew. I thought all these 'natural' supplements were magically better because they’re in glass bottles with cursive font. Guess I’ll go back to reading the tiny print instead of trusting marketing.
brooke wright
January 26, 2026 AT 03:04I took 3 different things last week and now I’m dizzy and my heart is racing. I didn’t know melatonin and diphenhydramine were both sedatives. I thought I was just being sleepy. Can someone tell me what to do? I’m scared. I don’t know who to ask.
Nick Cole
January 26, 2026 AT 09:32I used to think the expiration date was just a suggestion. Then I found a 10-year-old bottle of ibuprofen in my drawer. I threw it out. But now I keep a little calendar on my fridge to track when things expire. It’s weirdly satisfying to check them off. Like a little life hack.