Codeine Conversion Calculator
How Codeine Works
Codeine is a prodrug that requires conversion to morphine by the CYP2D6 enzyme. Only 5-10% of codeine becomes active morphine. Fluoxetine and paroxetine block this conversion.
Calculate Your Morphine Conversion
Your Results
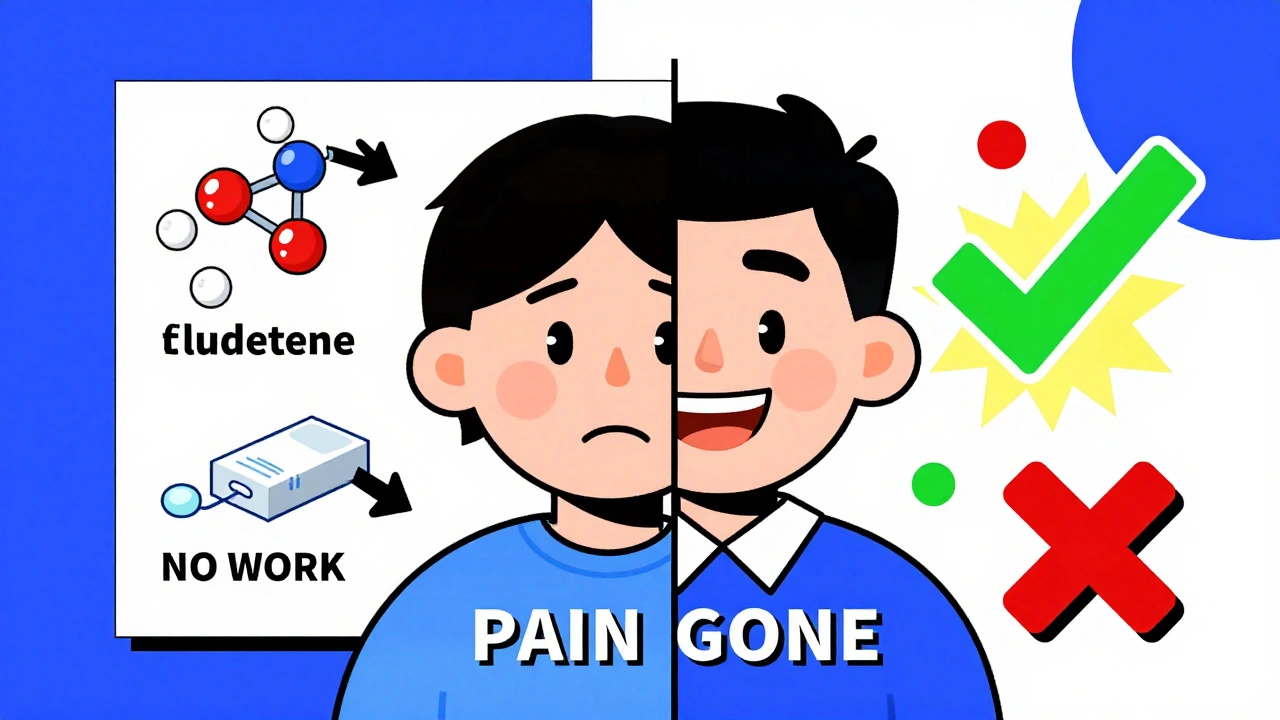
Have you ever taken codeine for pain and felt like it did absolutely nothing? You followed the dose, waited the right amount of time, and still felt the same ache. If you’re also taking fluoxetine or paroxetine - common antidepressants sold as Prozac or Paxil - that’s not a coincidence. It’s a well-documented, clinically significant drug interaction that shuts down codeine’s pain-relieving power. And it’s happening more often than most doctors realize.
How Codeine Actually Works (Spoiler: It’s Not What You Think)
Codeine isn’t the painkiller itself. It’s a prodrug - meaning your body has to turn it into something else to make it work. That something else is morphine. And the enzyme responsible for this conversion? CYP2D6. This liver enzyme does one specific job: it removes a methyl group from codeine, turning it into morphine. Without that step, codeine is basically useless for pain relief.
Only about 5 to 10% of a codeine dose becomes morphine. That’s why even when it works, the pain relief isn’t as strong as with other opioids. But when CYP2D6 gets blocked, that 5-10% drops to near zero. And that’s exactly what happens when you take fluoxetine or paroxetine alongside codeine.
Why Fluoxetine and Paroxetine Are the Worst Culprits
Not all antidepressants mess with codeine. Among SSRIs, fluoxetine and paroxetine are the strongest CYP2D6 inhibitors. Paroxetine is especially powerful - it binds to the enzyme so tightly that it can reduce morphine production by up to 85%. Fluoxetine isn’t far behind, cutting morphine levels by around 78%. These aren’t small effects. They’re total shutdowns.
Compare that to other SSRIs: sertraline only cuts CYP2D6 activity by about 60%, and citalopram or escitalopram barely touch it. So if you’re on an SSRI and need pain relief, switching from fluoxetine or paroxetine to citalopram could mean the difference between feeling nothing and getting real relief from codeine.
Studies back this up. In one trial, people taking 20 mg of paroxetine daily for a week had their morphine levels from codeine drop by 83%. Their pain relief? Cut by 62%. That’s not a minor reduction. That’s a complete failure of the drug to do its job.
The FDA and Global Health Agencies Have Warned About This
This isn’t some obscure theory. The U.S. Food and Drug Administration (FDA) issued a formal warning in 2007 and strengthened it in 2012. Their message? Strong CYP2D6 inhibitors like fluoxetine and paroxetine can make codeine ineffective. The European Medicines Agency (EMA) says the same. And the Clinical Pharmacogenetics Implementation Consortium (CPIC), which sets global standards for genetic drug use, explicitly says: avoid codeine if you’re taking these drugs.
Even more telling? The FDA’s own table on codeine therapy lists fluoxetine and paroxetine as inhibitors that reduce CYP2D6 activity. They don’t just mention it - they put it in writing for every prescriber to see.
Real Patients, Real Stories
Doctors aren’t just reading about this - they’re seeing it every day.
A 2020 survey of over 1,200 pain specialists found that nearly 8 out of 10 had treated a patient whose codeine didn’t work because of an SSRI. Paroxetine was named most often, followed by fluoxetine. One anesthesiologist shared a case: a woman after hysterectomy got standard codeine doses but reported zero pain relief. Switched to oxycodone? Immediate relief. No change in dose. Just a different opioid.
Pharmacists are seeing it too. On Reddit’s r/Pharmacy, users report the same pattern: patients on Paxil or Prozac come in confused because codeine isn’t helping. The answer? Always switch to hydrocodone or oxycodone - opioids that don’t rely on CYP2D6.
The FDA’s adverse event database has 247 reports of inadequate pain control with codeine and paroxetine combinations. That’s not a fluke. It’s a pattern. And the odds of this happening are more than 12 times higher than expected.
What to Use Instead of Codeine
If you’re on fluoxetine or paroxetine and need pain relief, codeine is off the table. But you still have options - and they’re better than you think.
Oxycodone is metabolized mainly by CYP3A4, not CYP2D6. That means fluoxetine and paroxetine don’t touch it. It’s a direct-acting opioid, so no conversion needed. Same goes for hydromorphone and morphine - both are already active and bypass CYP2D6 entirely.
Hydrocodone is another option, though it does have a minor CYP2D6 pathway. But its main effect comes from its own activity, so even with inhibition, it still works reasonably well. That’s why it’s often preferred over codeine in patients on SSRIs.
And if you’re on fluoxetine or paroxetine for depression, consider switching your antidepressant. Citalopram or escitalopram don’t interfere with CYP2D6. You can keep your mental health treatment and get real pain relief.
Testing Can Help - But You Don’t Always Need It
Some hospitals now test patients for CYP2D6 genetics before prescribing opioids. That’s great for people with rare genetic variants - like ultrarapid metabolizers who turn codeine into too much morphine and risk overdose. But for most people on fluoxetine or paroxetine, the problem isn’t genetics. It’s the drug interaction.
You don’t need a DNA test to know you’re at risk. If you’re taking Prozac or Paxil and codeine isn’t working, the answer is already clear. Don’t wait for a test. Switch the opioid.
Still, if you’re on long-term opioid therapy and antidepressants, genetic testing can help avoid future issues. A 2023 clinical trial showed that using genetic data to guide opioid choice reduced treatment failures by 57%.
Why This Interaction Is Getting Worse - And What’s Changing
Codeine prescriptions in the U.S. have dropped by over 40% since 2010. Why? One major reason: doctors are learning this interaction. More than a third of prescribing changes were directly linked to concerns about CYP2D6 inhibitors.
Hospitals are catching on too. A pilot program in 15 U.S. hospitals found that when pharmacists started checking for CYP2D6 inhibitors before dispensing codeine, they prevented over 1,800 treatment failures in just six months.
Electronic health records are starting to flag these interactions. Epic Systems, one of the biggest EHR vendors, added CYP2D6 decision support in late 2023. That means when a doctor tries to prescribe codeine to someone on paroxetine, the system will pop up a warning.
And the cost of testing is falling. Studies show that screening for CYP2D6 before prescribing codeine is cost-effective - it saves money by avoiding failed treatments, repeat visits, and unnecessary dose increases.
What You Should Do Right Now
If you’re taking fluoxetine or paroxetine and your doctor just prescribed codeine:
- Don’t take it. It won’t work.
- Call your doctor or pharmacist. Say: “I’m on [medication]. Will codeine still work?”
- Ask for oxycodone, hydromorphone, or morphine instead.
- If you’re open to switching antidepressants, ask about citalopram or escitalopram.
If you’re already taking codeine and it’s not helping - and you’re on one of these SSRIs - you’re not imagining it. The science is clear. Your pain isn’t worse. The drug is broken for you.
This isn’t about being “resistant.” It’s about biology. And now that you know, you can fix it.


10 Comments
Deborah Andrich
December 12, 2025 AT 18:45This is life-saving info. I was on paroxetine for years and got codeine after surgery and felt nothing. My doctor acted like I was exaggerating. Turns out I wasn't - it was the drug interaction. I switched to oxycodone and finally slept through the night.
Why isn't this taught in med school?
Tommy Watson
December 13, 2025 AT 10:41bro codeine is just sugar pills if ur on prozac lmao i thought i was just weak af
Karen Mccullouch
December 15, 2025 AT 09:12Of course the FDA cares about this now. They waited until Big Pharma stopped pushing codeine like it was candy. Meanwhile, my grandma died because her doctor didn't know this. USA still treats patients like lab rats.
And don't get me started on how they let Paxil be sold like it's harmless.
Corporate greed kills. Always.
Michael Gardner
December 15, 2025 AT 18:03Actually, the CYP2D6 pathway isn't the only reason codeine fails. Some people metabolize it poorly regardless of SSRIs. And oxycodone isn't always better - it's more addictive. You're oversimplifying a complex pharmacology issue.
Also, morphine is still the gold standard for severe pain. Why not just use that?
Ronan Lansbury
December 16, 2025 AT 01:56Let me guess - this was funded by Purdue Pharma or some opioid lobby. The FDA doesn't care about patient outcomes. They care about lawsuits. And CYP2D6 testing? That's just a Trojan horse for genetic surveillance.
Next they'll be scanning your DNA before you can buy aspirin.
Wake up, sheeple.
Jade Hovet
December 17, 2025 AT 12:27OMG I’ve been through this!! 😭 I was on Prozac and got codeine for a tooth extraction… zero pain relief. My dentist was so confused. I cried in the parking lot. Then I switched to citalopram and now I can take oxycodone without issue. Thank you for posting this - I needed to know I wasn’t crazy 🙏💖
Also, if anyone needs a good pharmacy to talk to, DM me - I’ll send you the script template I used!
nithin Kuntumadugu
December 18, 2025 AT 13:42lol this is just another western medical scam. In India we use turmeric and ashwagandha for pain. Codeine is just a colonial drug anyway. Your body is weak because you eat processed food and sit all day. No wonder you need opioids. Try yoga.
Also, CYP2D6? Sounds like a CIA code name.
John Fred
December 19, 2025 AT 15:15As a clinical pharmacist, I see this daily. The key is knowing which opioids are CYP2D6-independent: morphine, hydromorphone, oxycodone (primary pathway is CYP3A4). Hydrocodone is a gray zone - works fine for most, but if you're a poor metabolizer AND on paroxetine, you might still underrespond.
Pro tip: Always check the metabolic pathway before prescribing. And yes, citalopram/escitalopram are safer SSRIs for pain patients. I’ve switched 47 patients in the last year. All improved.
Also, EHR flags are finally useful. Thank you, Epic.
Harriet Wollaston
December 21, 2025 AT 01:21I’m so glad someone finally wrote this. I’ve been on Paxil for 8 years and just assumed I was ‘high tolerance’ to pain meds. I had to get my knee replaced last year and the surgeon gave me codeine. I was in tears from pain and he kept upping the dose. I almost refused the surgery because I was so scared of being in pain again.
Switched to citalopram last month and now I’m on oxycodone - I can walk without screaming. This isn’t just science - it’s dignity.
Thank you for making this clear. I’m sharing this with every friend on antidepressants.
Tyrone Marshall
December 22, 2025 AT 14:49This is a beautiful example of how biology doesn't care about our assumptions. We assume drugs work the same for everyone - but the human body is a complex, evolving system shaped by genetics, environment, and chemistry. Codeine isn't broken. It's just not for everyone.
And the real tragedy isn't the interaction - it's that this knowledge is still not universal in medical practice. We treat patients as if they're interchangeable parts, not unique biological systems.
What if we stopped prescribing based on protocols and started prescribing based on individual biochemistry? That’s not just medicine - that’s respect.
And yes, switching SSRIs is a valid option. It’s not weakness. It’s adaptation. We do it with diet, exercise, therapy - why not meds?