When your liver is damaged by cirrhosis, fluid doesn’t just sit where it should-it leaks into your belly. This is ascites, and it’s not just uncomfortable. It’s a sign your liver is failing. About half of people with cirrhosis will develop ascites within 10 years, and once it shows up, your chances of living another two years drop to 50%. That’s not a scare tactic-it’s what the American Association for the Study of Liver Diseases says. The good news? You can manage it. The tricky part? The rules have changed, and doctors aren’t all on the same page anymore.
Why Fluid Builds Up in Your Belly
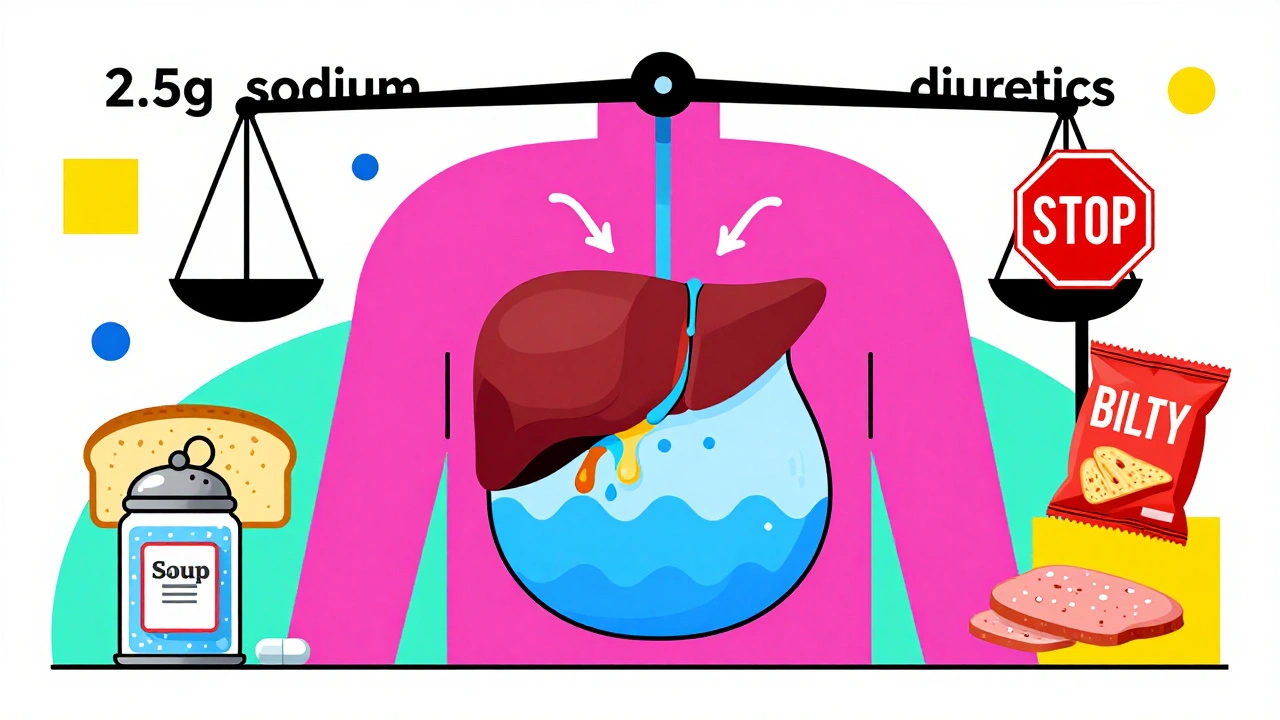
It starts with high pressure in the veins around your liver. This pressure forces fluid out of your blood vessels and into your abdomen. But here’s the twist: your kidneys don’t just let it go. They start holding onto sodium and water like they’re running out of supply. That’s because your body thinks your blood volume is low-even though there’s fluid pooling in your belly. It’s a cruel trick. Your liver can’t filter toxins, your kidneys can’t flush fluid, and your body keeps making the problem worse.The Old Rule: Eat Less Salt
For decades, the go-to advice was simple: cut salt to under 2 grams a day. That’s less than a teaspoon of table salt. The logic? Less sodium means less fluid retention. It sounds straightforward. But here’s the catch: most of the sodium you eat doesn’t come from the salt shaker. It’s in bread, canned soup, deli meats, sauces, and packaged snacks. Trying to hit under 2 grams a day means reading every label, cooking everything from scratch, and avoiding restaurants entirely. Studies show fewer than 4 in 10 people can stick to it.The New Debate: Is Salt Really the Enemy?
Recent studies are flipping the script. In 2022, a major trial found that patients with ascites who ate 5-6.5 grams of salt per day (about 2-2.5 grams of sodium) actually had less fluid buildup than those on strict low-salt diets. Their ascites resolved in 45% of cases-nearly three times higher than the 16% who followed the old 2-gram rule. Why? Because when you cut salt too hard, your kidneys go into survival mode. They slow down blood flow to the kidneys, which can trigger something even worse: hepatorenal syndrome. That’s when kidney function crashes, and survival drops to under 6 months. Dr. Pere Gines, who led that 2022 study, says strict salt restriction might actually hurt more than help. He’s not saying eat pizza every day. He’s saying: don’t panic. Moderate salt intake-with the right diuretics-works better than extreme restriction.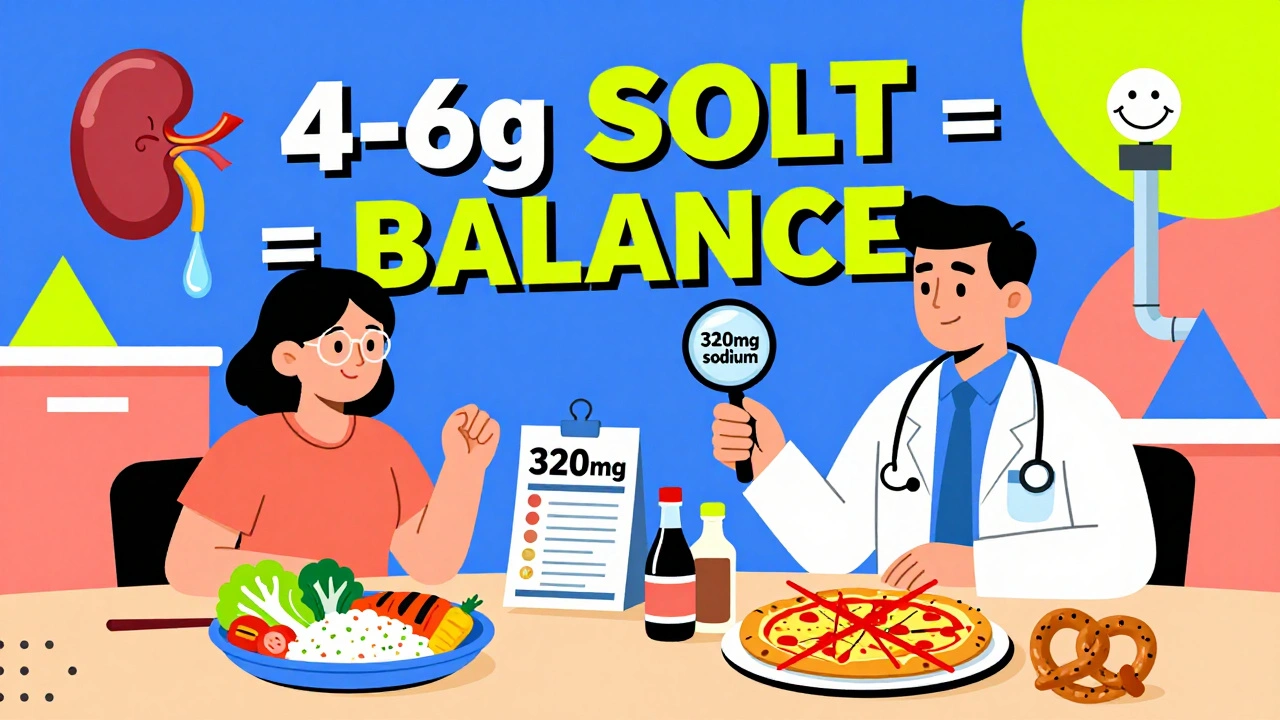
Diuretics: The Real Workhorses
Salt restriction alone won’t fix ascites. Diuretics do. The two main ones are spironolactone and furosemide. Spironolactone is the first-line drug. You start at 100 mg a day, and your doctor will bump it up every 3 days-up to 400 mg-if needed. It works by blocking the hormone that tells your kidneys to hang onto sodium. Furosemide comes in second. You start at 40 mg a day, maxing out at 160 mg. It’s stronger and faster, but it can mess with your electrolytes if used alone. Together, they’re powerful. About 90% of people with simple ascites see improvement when both are used correctly. But there’s a catch: you can’t rush it. Your doctor will want you to lose no more than 0.5 kg (1 pound) per day if you don’t have swollen legs, and 1 kg (2 pounds) if you do. Lose weight too fast, and you risk kidney failure or low blood pressure.What to Watch For: Hyponatremia and Drug Risks
About 1 in 3 people with ascites have low sodium in their blood-hyponatremia. That doesn’t mean you need more salt. It means your body is holding onto too much water. If your sodium drops below 130, your doctor will adjust your diuretics and may limit fluids. Never take NSAIDs like ibuprofen or naproxen. They can crash your kidney function. Same with ACE inhibitors and ARBs-blood pressure meds that sound harmless but can speed up kidney damage in cirrhosis. One study found these drugs triple the risk of needing dialysis.When Diuretics Don’t Work
About 1 in 10 people don’t respond to diuretics, even at max doses. That’s called refractory ascites. If you’re in this group, your only real option is a procedure called large-volume paracentesis. A needle is inserted into your belly to drain the fluid-up to 5 liters at a time. But here’s the catch: you need to get an IV infusion of albumin afterward. Without it, your blood pressure drops, and your kidneys can fail. This isn’t a cure-it’s a rescue. It needs to be done in a hospital, and it carries a 5-10% risk of infection or bleeding.
What About Other Treatments?
There are drugs called vaptans that block water retention. They sound perfect. But they cost $5,000 to $7,000 per course-and you can only use them for 30 days. They’re not for long-term use. Transplant is the only cure, but not everyone qualifies. For now, diuretics and smart sodium intake are your best tools.The Middle Ground: A Practical Approach
So what should you do? Don’t go full keto on salt. Don’t eat a bag of chips a day. Aim for 4-6 grams of salt total per day-that’s about one and a half teaspoons. Focus on whole foods: fresh meat, vegetables, fruits, rice, beans. Avoid processed stuff. Read labels. If a food has more than 300 mg of sodium per serving, skip it. Cook at home. Use herbs, lemon, vinegar instead of salt. And never stop your diuretics without talking to your doctor. Even if you feel better, stopping them suddenly can make fluid come back fast. Your doctor will check your blood sodium at least twice a week when you start. That’s not overkill-it’s essential.What’s Coming Next?
A big trial called PROMETHEUS is underway, comparing strict salt restriction with no restriction in cirrhosis patients. Results are due by the end of 2025. Until then, the debate continues. But one thing is clear: ascites management isn’t about following a rigid rule. It’s about balance. Your liver is weak. Your kidneys are stressed. Your body is trying to survive. The goal isn’t perfection-it’s control. Enough salt to keep your kidneys working. Enough diuretics to drain the fluid. And enough monitoring to catch trouble before it’s too late.How much sodium should I really eat if I have ascites?
Current guidelines say under 2 grams per day, but newer research suggests 2-2.5 grams (4-6 grams of salt) works better for most people, especially when paired with diuretics. Strict restriction often fails because it’s hard to follow and can hurt kidney function. Talk to your doctor about what’s right for you based on your blood tests and symptoms.
Can I still eat out or have snacks with ascites?
Yes-but you need to be smart. Avoid fast food, canned soups, deli meats, soy sauce, and packaged snacks. Ask for meals without added salt. Choose grilled chicken or fish with steamed vegetables. Opt for fresh fruit instead of chips. A single serving of canned tuna can have over 500 mg of sodium. A slice of bread? Around 200 mg. Track it. Your daily limit isn’t zero-it’s about 2,000 mg max.
Why do I need to check my blood sodium so often?
Diuretics can make your sodium levels drop too low, especially if you’re also drinking too much water. Low sodium (below 130) can cause confusion, seizures, or coma. Your doctor checks it twice a week at first to make sure your treatment isn’t pushing you into danger. If your sodium drops, they’ll adjust your meds-not add salt.
What happens if I stop taking my diuretics?
Fluid will come back-fast. Diuretics don’t cure ascites; they manage it. Stopping them, even if you feel fine, can cause your belly to swell again within days. If you’re having side effects like dizziness or cramps, tell your doctor. Don’t quit on your own. There are ways to adjust the dose or switch medications safely.
Are there any foods I should avoid completely?
Yes. Avoid processed meats (bacon, ham, sausages), canned vegetables and soups, pickled foods, soy sauce, teriyaki, bottled salad dressings, and most restaurant meals. Also skip salted nuts, pretzels, and cheese with added salt. Read labels. If sodium is listed as more than 300 mg per serving, it’s too high. Choose fresh or frozen without added sauce.
Can I drink alcohol if I have ascites?
No. Alcohol directly damages your liver and makes ascites worse. Even small amounts can trigger fluid buildup or cause sudden liver failure. If you’ve been drinking, stopping now is the single most important thing you can do to slow your disease. Your doctor will test your liver function regularly to track progress.
How do I know if my ascites is getting worse?
Watch for rapid weight gain (more than 1 kg in 2 days), increasing belly size, shortness of breath, swelling in your legs or ankles, or feeling full after eating just a little. These mean fluid is building up again. Call your doctor right away. You might need a bigger dose of diuretics or a paracentesis.

9 Comments
Steve Sullivan
December 7, 2025 AT 22:03bro i was told to go zero salt and nearly passed out from dizziness. my doc finally said 4-6g salt is fine if i’m on spironolactone. my belly’s been flat for 3 months now. 🙌
Simran Chettiar
December 8, 2025 AT 20:08It is, perhaps, a profound irony that our modern medical paradigm, steeped in reductionist dogma, has for decades prescribed a dietary regimen that, while theoretically sound, fails to account for the intricate neurohormonal dysregulation inherent in cirrhotic ascites. The body does not operate on binary rules of ‘less is better’-it operates on homeostatic survival mechanisms that, when violently disrupted, precipitate hepatorenal syndrome. The 2022 Gines trial, therefore, does not merely challenge convention-it illuminates a deeper truth: medicine must evolve beyond the tyranny of arbitrary thresholds.
Anna Roh
December 10, 2025 AT 09:38lol so we’re just gonna eat chips now? 🤡
Richard Eite
December 11, 2025 AT 22:31US doctors know what theyre doing. europeans are still stuck in 1990s thinking. 2g salt? thats for weaklings. 5g is the new standard. period
Katherine Chan
December 12, 2025 AT 07:05this is actually so hopeful. i thought i had to give up everything i loved but this makes it feel doable. small changes, not perfection. you got this 💪
Philippa Barraclough
December 13, 2025 AT 11:58The paper referenced from Gines et al. (2022) was a multicenter, randomized controlled trial with a cohort of 217 patients, stratified by baseline sodium levels and renal function. The primary endpoint was time to resolution of ascites within 12 weeks, with secondary outcomes including incidence of hyponatremia and hospitalization rates. Notably, the moderate-sodium group demonstrated a statistically significant reduction in ascites volume (p<0.01) without increased incidence of renal impairment, suggesting that the traditional sodium restriction protocol may be unnecessarily restrictive in patients with preserved glomerular filtration rate. However, the authors caution that these findings are not generalizable to those with advanced hepatorenal syndrome or uncontrolled hypertension.
Tim Tinh
December 15, 2025 AT 06:39man i used to cook everything from scratch but honestly? just avoid the processed junk and you’re 80% there. fresh chicken, rice, veggies. no soy sauce. lemon and garlic = magic. and dont skip your diuretics. i learned that the hard way 😅
Olivia Portier
December 16, 2025 AT 00:06i had ascites for 2 years and thought i was doomed. then my nurse practitioner sat with me and said 'you don’t need to be perfect, you need to be consistent.' i started reading labels, cooking once a week, and taking my meds like clockwork. my belly shrunk. i’m alive. you can too. we’re in this together ❤️
Tiffany Sowby
December 17, 2025 AT 11:10why do doctors even bother with this? everyone knows the real solution is a liver transplant. until then, it’s just a waiting game with a side of salt shaming. i’m tired of being told what to eat when my liver is already dying. 🙄