Every year, nearly one in four older adults falls. For many, it’s not just a stumble-it’s a broken hip, a hospital stay, or worse. And surprisingly, one of the most common culprits isn’t loose rugs or poor lighting. It’s a medication many older adults take daily without realizing the danger: first-generation sedating antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and brompheniramine. These drugs are sold over-the-counter, labeled as sleep aids or allergy relievers, and often taken without a doctor’s approval. But for people over 65, they’re a hidden fall risk-and the science is clear.
Why Sedating Antihistamines Are Dangerous for Older Adults
First-generation antihistamines were designed in the 1940s to block histamine and stop allergy symptoms. But unlike modern versions, they don’t stop at the nose or throat. They cross the blood-brain barrier easily, messing with brain chemistry. This causes drowsiness, slowed reaction time, dizziness, and poor balance-all of which make falls more likely.Older bodies process these drugs differently. A healthy 30-year-old might clear diphenhydramine in about 8.5 hours. But in someone over 65, that time stretches to 13.5 hours or more. That means the sedative effect lingers longer, often into the next day. One study found that 8% of older adults who filled a prescription for these meds fell within 60 days. That’s not rare. That’s common.
The American Geriatric Society calls these drugs “potentially inappropriate” for seniors in their Beers Criteria. Why? Because they don’t just cause sleepiness. They trigger confusion, dry mouth, constipation, blurred vision, and even delirium in hospitalized patients. One study showed older adults on these meds were 2.3 times more likely to experience delirium during a hospital stay. That’s not a side effect-it’s a crisis waiting to happen.
The Numbers Don’t Lie
Data from the CDC shows over 36 million falls happen each year among U.S. adults 65 and older. More than 32,000 of those result in death. And according to a 2025 study in the Journal of the American Geriatrics Society, nearly one-third of older adults who visited a doctor for dizziness had filled a prescription for a vestibular suppressant-most of them first-gen antihistamines.A 2018 meta-analysis in Osteoporosis International looked at 190,000 older adults and found a 54% higher risk of injurious falls and a 43% higher risk of fractures linked to these drugs. That’s not a small bump. That’s a massive spike. Even more telling: second-generation antihistamines like loratadine, cetirizine, and fexofenadine showed no increased fall risk in the same studies. The difference isn’t subtle. It’s life-or-death.
Why do people keep using them? Because they’re cheap, easy to buy, and marketed as harmless. Diphenhydramine alone sold 28.7 million units in 2024 to seniors in the U.S. That’s $142 million in sales. But sales don’t equal safety. The FDA added warnings to OTC labels in 2020, but they’re buried in small print. Most seniors don’t read them. Or they don’t realize their “sleep aid” is the same drug that’s making them wobbly.
Second-Generation Antihistamines: The Safer Choice
Not all antihistamines are created equal. Second-generation options like fexofenadine (Allegra), loratadine (Claritin), and cetirizine (Zyrtec) were designed to stay out of the brain. They’re just as good at stopping sneezing and itchy eyes-but they don’t make you feel like you’ve had three glasses of wine at noon.Here’s the key difference: anticholinergic burden. First-gen antihistamines score 3 or 4 on the Anticholinergic Cognitive Burden Scale. That’s the highest level-strong enough to mess with memory and movement. Second-gen drugs score 0 or 1. Minimal to none. A 2025 study found that switching from diphenhydramine to fexofenadine cut fall risk by 42%.
That doesn’t mean second-gen drugs are risk-free. Cetirizine still causes drowsiness in about 14% of older adults. Fexofenadine? Only 6%. So if you need an antihistamine, fexofenadine is the safest bet. Loratadine is close behind. Avoid cetirizine if you’re already unsteady on your feet.
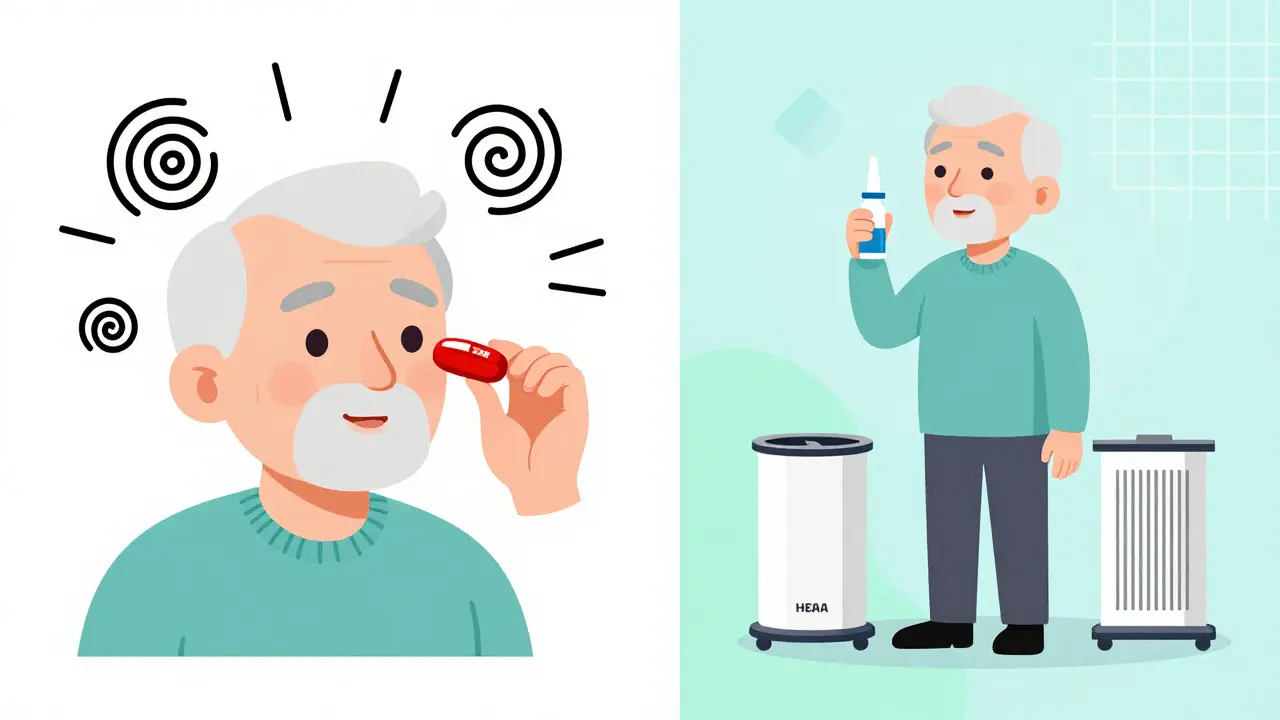
What to Do Instead of Taking the Pill
The best way to avoid a fall isn’t to switch drugs-it’s to skip the drugs altogether. For allergies, there are powerful non-medication options:- Nasal saline irrigation reduces allergy symptoms by 35-40%, according to a 2022 study in JAMA Otolaryngology.
- Allergen-proof bedding cuts dust mite exposure by 83%.
- HEPA air filters remove 99.97% of airborne allergens from the air.
For sleep, don’t reach for Benadryl. The American Geriatric Society specifically warns against using it for insomnia in seniors. Instead, try:
- Keeping a consistent sleep schedule-even on weekends
- Avoiding caffeine after noon
- Turning off screens an hour before bed
- Making the bedroom cool, dark, and quiet
These aren’t magic tricks. They’re proven, safe, and free. And they don’t make you stumble when you get up to use the bathroom at night.
How to Talk to Your Doctor or Pharmacist
If you or a loved one is taking a first-generation antihistamine, don’t stop cold turkey. Talk to a professional. Ask these questions:- Is this medication still necessary?
- Can we switch to a safer alternative like fexofenadine or loratadine?
- What’s the lowest dose I can take?
- Can we try non-drug options first?
Pharmacists are your allies. Many offer “brown bag reviews”-where you bring in all your pills, supplements, and OTC meds. On average, they find 3.2 high-risk medications per patient. That’s not a failure. That’s an opportunity to get safer.
The CDC’s STEADI program recommends a simple three-step plan: STOP high-risk meds when possible, SWITCH to safer ones, and REDUCE doses to the minimum needed. It’s not about cutting everything-it’s about cutting the things that could kill you.

Make Your Home Safer While You Adjust
Even if you switch medications, your home might still be a hazard. Falls aren’t just about drugs-they’re about environment. Simple changes cut risk dramatically:- Install grab bars in the shower and next to the toilet-reduces falls by 28%
- Improve lighting in hallways and stairs-reduces falls by 32%
- Remove loose rugs and clutter from walkways
- Add non-slip mats in the bathroom
- Keep a flashlight by the bed for nighttime trips
These fixes cost less than a month’s supply of Benadryl. And they last years.
What’s Changing in 2026
The tide is turning. Since 2024, Medicare’s Annual Wellness Visit now requires doctors to document a review of high-risk medications-including sedating antihistamines. The CDC updated its STEADI toolkit in January 2025 with a new medication risk module. And the American Academy of Neurology now advises doctors to avoid these drugs entirely in patients with a history of falls.Even better, two new antihistamines are in Phase II trials-AGS-2025-01 and FEX-AGE-101. Early results show an 89% reduction in drowsiness compared to diphenhydramine. They’re not on the market yet, but they signal a future where allergy and sleep meds don’t come with a fall risk.
For now, the solution is simple: know what you’re taking. Ask questions. Switch to safer options. Use non-drug tools. And make your home safer. These steps won’t just prevent falls-they can keep you living independently, safely, and without fear.
Are over-the-counter antihistamines safe for seniors?
No, first-generation OTC antihistamines like diphenhydramine (Benadryl) and chlorpheniramine are not safe for older adults. They significantly increase fall risk due to drowsiness, dizziness, and impaired balance. Even though they’re sold without a prescription, they carry the same risks as prescription sedatives. Second-generation antihistamines like fexofenadine and loratadine are much safer alternatives.
What’s the safest antihistamine for seniors?
Fexofenadine (Allegra) is the safest choice for seniors. It has minimal sedative effects and no anticholinergic activity. Loratadine (Claritin) is also a good option. Cetirizine (Zyrtec) is less ideal-it causes drowsiness in about 14% of older adults. Avoid diphenhydramine, chlorpheniramine, and brompheniramine entirely.
Can I stop taking diphenhydramine cold turkey?
It’s not recommended. If you’ve been using diphenhydramine regularly-especially for sleep-stopping suddenly can cause rebound symptoms like worse allergies or insomnia. Talk to your doctor or pharmacist first. They can help you taper off slowly and replace it with safer strategies like sleep hygiene or nasal irrigation.
How long does diphenhydramine stay in an older adult’s system?
In healthy adults, diphenhydramine clears in about 8.5 hours. But in older adults, it can take up to 13.5 hours or longer due to slower metabolism. The sedative effects can last 6-8 hours, meaning someone who takes it at night may still feel groggy the next morning-increasing fall risk during daily activities.
Why do doctors still prescribe these drugs if they’re dangerous?
Many doctors aren’t aware of the updated guidelines, or they assume OTC means safe. Others prescribe them because patients ask for them-especially for sleep. There’s also a gap between research and practice: studies show first-gen antihistamines are prescribed at similar rates to younger patients, even though the risks are much higher in seniors. Education and medication reviews are helping close this gap.
Can I use natural remedies instead of antihistamines?
Yes. For allergies, saline nasal rinses reduce symptoms by 35-40%, allergen-proof bedding cuts dust mites by 83%, and HEPA filters remove 99.97% of airborne allergens. For sleep, focus on sleep hygiene: regular bedtime, no screens before bed, cool dark room, and avoiding caffeine after noon. These methods are effective, safe, and don’t carry fall risks.


1 Comments
Sandeep Kumar
February 2, 2026 AT 08:27These meds are a joke for seniors and everyone knows it except the doctors who still push them like candy