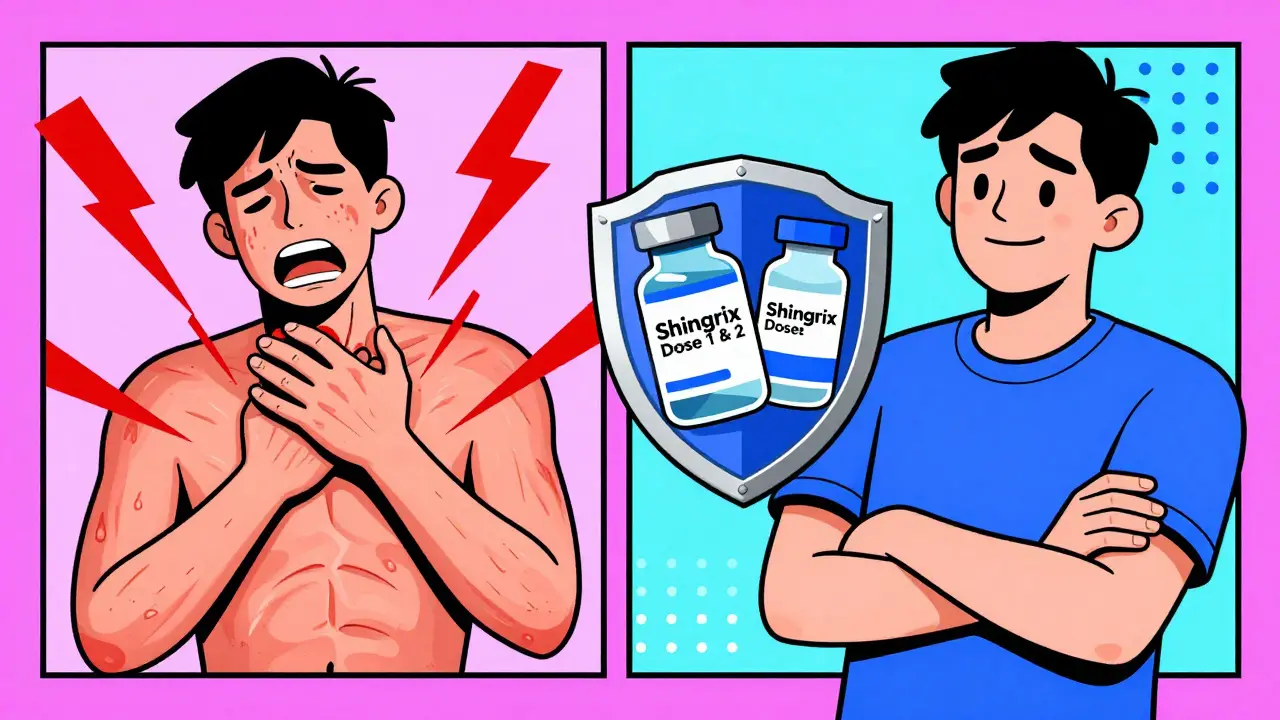
Shingles isn’t just a rash. For many people, it’s months of burning pain that won’t go away-even after the blisters heal. That’s the reality of postherpetic neuralgia, the most common and cruel complication of shingles. And it’s not something that only affects the elderly. About 1 in 3 people in the U.S. will get shingles in their lifetime. The good news? There’s a vaccine that works better than anything we’ve ever had. It’s called Shingrix, and if you’re over 50, or even younger with certain health conditions, you need to know exactly who should get it and when.
Who Really Needs the Shingles Vaccine?
You don’t have to be 70 to be at risk. The CDC recommends Shingrix for everyone 50 and older, no matter if you’ve had shingles before or think you’re healthy. Why? Because once you’ve had chickenpox-and almost everyone has-the virus stays hidden in your nerves. It can wake up decades later, triggered by stress, aging, or a weakened immune system.
But here’s the key detail most people miss: if you’re 19 or older and immunocompromised, you should also get Shingrix. That includes people with diabetes, cancer, HIV, or those taking medications like steroids, chemotherapy, or biologics for autoimmune diseases. Unlike the old vaccine (Zostavax), Shingrix doesn’t contain live virus. That means it’s safe for people with weak immune systems. In fact, the CDC updated its guidelines in 2023 to make it clear: if you’re immunocompromised, you’re not just eligible-you’re a top priority.
Even if you got Zostavax years ago, you still need Shingrix. The old vaccine offered only about half the protection, and it wore off quickly. Shingrix gives you over 90% protection for at least seven years, even into your 70s and 80s. There’s no reason to wait.
When Should You Get It?
Shingrix isn’t a one-shot deal. It’s two doses, given 2 to 6 months apart. That’s non-negotiable. The first dose starts your protection. The second dose locks it in. Skip it, and you’re leaving yourself vulnerable.
For most people, the ideal window is 2 to 6 months between doses. But if you’re immunocompromised, you can get the second dose as early as 1 month after the first. That’s a critical exception. If you’re about to start chemotherapy or a new immunosuppressant, talk to your doctor. Getting the second dose sooner can make a big difference in how well you’re protected before your immune system drops.
There’s one hard rule: don’t give the second dose before 4 weeks. If you accidentally get it too early, you’ll need to repeat it. That’s not a mistake you want to make. Pharmacies and clinics now use automated reminders to help people stay on track, but you still need to keep your own calendar. Write it down. Set a phone alert. Don’t rely on memory.
What About Side Effects?
Let’s be honest: Shingrix can make you feel awful-for a day or two. Around 78% of people get pain, redness, or swelling at the injection site. About 45% feel muscle aches. Nearly 40% get tired. Headaches, fever, and nausea are common too. These aren’t rare side effects. They’re the norm.
But here’s what most people don’t say: these reactions are a sign the vaccine is working. Your immune system is firing up. And compared to the pain of shingles? This is nothing. One man in his 60s told me he felt like he’d been hit by a truck after the second dose. He missed work for two days. But he’s had no shingles since. He says it was the best $220 he ever spent.
If you’re worried about side effects, schedule your shot on a Friday. Avoid planning big events, travel, or important meetings for the next 48 hours. Most people feel fine by day three. And if you’ve had a bad reaction to the first dose, you’ll likely have a milder one the second time. That’s been shown in multiple studies.
How Much Does It Cost?
Shingrix isn’t cheap. Each dose runs about $185 to $220 out-of-pocket. But if you’re on Medicare Part D, you pay nothing for the vaccine itself. The catch? You might still get hit with an administration fee-usually $20 to $40. That’s not covered by Part D, but many Medicare Advantage plans will cover it.
If you’re under 65 and have private insurance, check your plan. Most cover Shingrix fully under preventive care rules. If you’re uninsured, look into the Vaccines for Children program (if eligible) or patient assistance programs through GSK. Some pharmacies offer discounts. And if you’re on Medicaid, coverage varies by state-call ahead.
Don’t let cost stop you. Shingles can cost you thousands in medical bills, lost wages, and pain management. One study found the average out-of-pocket cost for treating shingles complications was over $4,000. Vaccination pays for itself.
What If You’ve Already Had Shingles?
You might think, ‘I’ve been through it once-I’m safe.’ That’s a dangerous myth. Shingles can come back. About 1 in 3 people who’ve had it get it again. And the second time? It can be worse.
The CDC says you can get Shingrix as soon as your rash has healed. No need to wait a year. No need to wait six months. Get it when you’re feeling better. The vaccine works whether you’ve had shingles or not. In fact, people who’ve had it often get the most benefit because their immune system is already primed to respond.
What About the Future?
There’s talk of a single-dose version of Shingrix in development. GSK is testing it in Phase II trials, and early results look promising. If it works, it could change everything-making it easier to get vaccinated, especially for older adults who struggle with follow-up appointments.
Right now, the push is to vaccinate earlier. The American Geriatrics Society now recommends talking to patients about Shingrix starting at age 50, not waiting until 65. Why? Because shingles risk climbs steadily after 50. The longer you wait, the more your immune system weakens. And the less protection you’ll get.
By 2030, one in five Americans will be over 65. That means millions more people at risk. Vaccination rates are rising-up from 34% in 2020 to 42% in 2023-but they’re still too low. The biggest barrier? Fear of side effects. Over 40% of unvaccinated adults say they’re scared of the reactions. But the data is clear: the side effects are temporary. The pain from shingles? Not.
What Happens If You Don’t Get It?
If you skip the vaccine, you’re rolling the dice. One in three people will get shingles. Of those, up to 1 in 5 will develop postherpetic neuralgia. That’s nerve pain that lasts months-or years. Some people can’t sleep. Can’t wear clothes. Can’t touch their own skin. Painkillers often don’t help. And there’s no cure.
Shingles can also lead to vision loss, hearing problems, brain inflammation, and even stroke. It’s not just a skin issue. It’s a neurological one. And it doesn’t care if you’re fit, healthy, or young. It only cares that you had chickenpox once.
Shingrix cuts your risk of shingles by more than 90%. It cuts your risk of long-term nerve pain by over 90% too. That’s not a small win. That’s life-changing protection.
Where Do You Go?
You don’t need a doctor’s appointment to get Shingrix. Pharmacies like CVS, Walgreens, and Walmart offer it. Most clinics, community health centers, and public health departments do too. Bring your insurance card. If you’re on Medicare, make sure they bill Part D. If you’re unsure, ask: ‘Do you give Shingrix? Is it covered under my plan?’
Don’t wait for your annual checkup. Go now. Schedule it. Get the first dose. Then set a reminder for the second. You’re not just protecting yourself-you’re protecting the people around you. Shingles isn’t contagious, but the virus can spread to someone who’s never had chickenpox. And if they get it? They’ll get chickenpox. Not shingles. Chickenpox. And that can be deadly for babies, pregnant women, or people with weak immune systems.

