Isotretinoin Depression Monitoring Schedule Calculator
Determine the appropriate depression monitoring phase based on treatment duration and PHQ-9 score thresholds
When doctors prescribe Isotretinoin a retinoid used for severe nodular acne that works by shrinking sebaceous glands and cutting sebum output, they must also think about the patient’s mind. The drug’s black‑box warning for birth defects is well known, but the debate over isotretinoin depression keeps clinicians on their toes. This guide walks you through the latest evidence, regulatory expectations, and day‑to‑day monitoring tactics so you can spot trouble early and act confidently.
Why the Psychiatric Question Matters
Acne can be emotionally crippling, and a clear skin outcome often lifts mood. At the same time, several large databases have flagged mood disturbances linked to isotretinoin. A 2025 analysis of the FDA Adverse Event Reporting System (FAERS) recorded 19,412 psychiatric reports from 12,312 users, with depression making up 47.5% of those events and a reporting odds ratio of 3.30 (95% CI 3.25‑3.35). Conversely, a 2023 JAMA Dermatology meta‑analysis of 24 studies found a 1‑year absolute depression risk of 3.83%-roughly the same as the general adolescent population.
Both numbers are real; they just come from different lenses. FAERS captures reported events, which can be influenced by heightened awareness, while meta‑analyses pool controlled studies that may miss rare signals. The takeaway? The absolute risk stays low, but the relative signal is strong enough to merit systematic monitoring.
Key Regulatory Frameworks
In the United States, the iPLEDGE program governs isotretinoin prescribing. Since the 2020 update, the program mandates monthly depression screening with the Patient Health Questionnaire‑9 (PHQ‑9) and requires a mental‑health evaluation if the score reaches 10 or higher. Australia’s Therapeutic Goods Administration (TGA) reinforced similar monitoring in March 2024, demanding documented psychiatric assessments for persistent symptoms. The European Medicines Agency (EMA) added a differential‑diagnosis flow in July 2023, asking clinicians to rule out vitamin B12 deficiency (present in about 19% of users) before attributing mood changes to the drug.
These rules converge on three core actions: baseline mental‑health assessment, scheduled follow‑ups during the high‑risk window (roughly weeks 1‑8), and clear red‑flag protocols for suicidal ideation or severe anxiety.
Evidence‑Based Monitoring Timeline
Multiple data sources point to a median onset of psychiatric symptoms around 80 days (≈ 11 weeks) after starting treatment. FAERS data show that 44% of reported events happen in the first eight weeks. Based on this, many clinics adopt a tiered schedule:
- Weeks 1‑4: weekly brief check‑ins (phone or secure messaging)
- Weeks 5‑8: bi‑weekly in‑person or video visits with PHQ‑9
- Weeks 9‑16: monthly visits, continue PHQ‑9
- Beyond week 16: quarterly mental‑health review until course ends (usually 15‑20 weeks)
Below is a concise snapshot you can print or embed in your clinic’s EMR.
| Period | Frequency | Tool | Trigger for Referral |
|---|---|---|---|
| Weeks 1‑4 | Weekly | Brief mood questionnaire | PHQ‑9 ≥10 or new suicidal thoughts |
| Weeks 5‑8 | Bi‑weekly | PHQ‑9 | Score increase ≥5 points or ideation |
| Weeks 9‑16 | Monthly | PHQ‑9 or Beck Depression Inventory | Any score ≥10 |
| Weeks 17‑end | Quarterly | PHQ‑9 | Persistent elevation |
Conducting the Baseline Assessment
Before the first pill, collect a comprehensive mental‑health snapshot:
- Ask about personal and family history of depression, bipolar disorder, or anxiety.
- Review current psychotropic medications and any recent changes.
- Administer a validated screen such as PHQ‑9 or the Beck Depression Inventory.
- Document the patient’s baseline mood, energy, sleep, and appetite.
- Explain the monitoring plan, emphasizing that the goal is early support, not to discourage treatment.
Patients with a prior psychiatric diagnosis should be flagged for more frequent visits and possibly a co‑managed approach with their primary mental‑health provider.
Red‑Flag Symptoms That Demand Immediate Action
Not every mood dip means the drug is the cause, but certain signs should trigger a stop‑and‑refer decision:
- Any expression of suicidal thoughts, plans, or intent.
- Severe anxiety that interferes with daily functioning and does not improve with standard coping strategies.
- Sudden, marked irritability or emotional blunting that contrasts sharply with the patient’s baseline.
- Psychotic features, such as hallucinations or delusions, though rare.
If any red flag appears, pause isotretinoin, arrange an urgent psychiatric evaluation, and consider alternative acne therapies (e.g., doxycycline, topical retinoids).
Alternative Acne Options and Their Psychiatric Profiles
When isotretinoin is halted, clinicians often turn to oral antibiotics like doxycycline or minocycline. Minocycline has been linked to depression in about 1.7% of users-a lower rate than the FAERS‑derived isotretinoin figures but still noteworthy. Topical retinoids (tretinoin, adapalene) lack systemic exposure and thus carry minimal psychiatric risk.
Choosing an alternative should weigh acne severity, patient preference, and any pre‑existing mental‑health conditions. A shared decision‑making conversation helps patients feel empowered and reduces anxiety about “giving up” a powerful acne solution.
Emerging Tools and Future Directions
Technology is tightening the monitoring loop. In August 2024 the FDA launched a pilot that syncs weekly digital PHQ‑9 entries directly into the iPLEDGE platform, flagging scores ≥10 for automatic clinician alerts. Early adopters report faster intervention times.
Genetic research is also promising. A July 2024 Journal of Clinical Psychiatry study identified the BDNF Val66Met polymorphism as a potential predictor of isotretinoin‑related depression, with 68% sensitivity. While not ready for routine use, such biomarkers could one day let doctors personalize monitoring intensity.
Finally, upcoming APA clinical practice guidelines (expected December 2024) will outline specific recommendations for patients with existing depression, reinforcing a move away from a one‑size‑fits‑all approach.
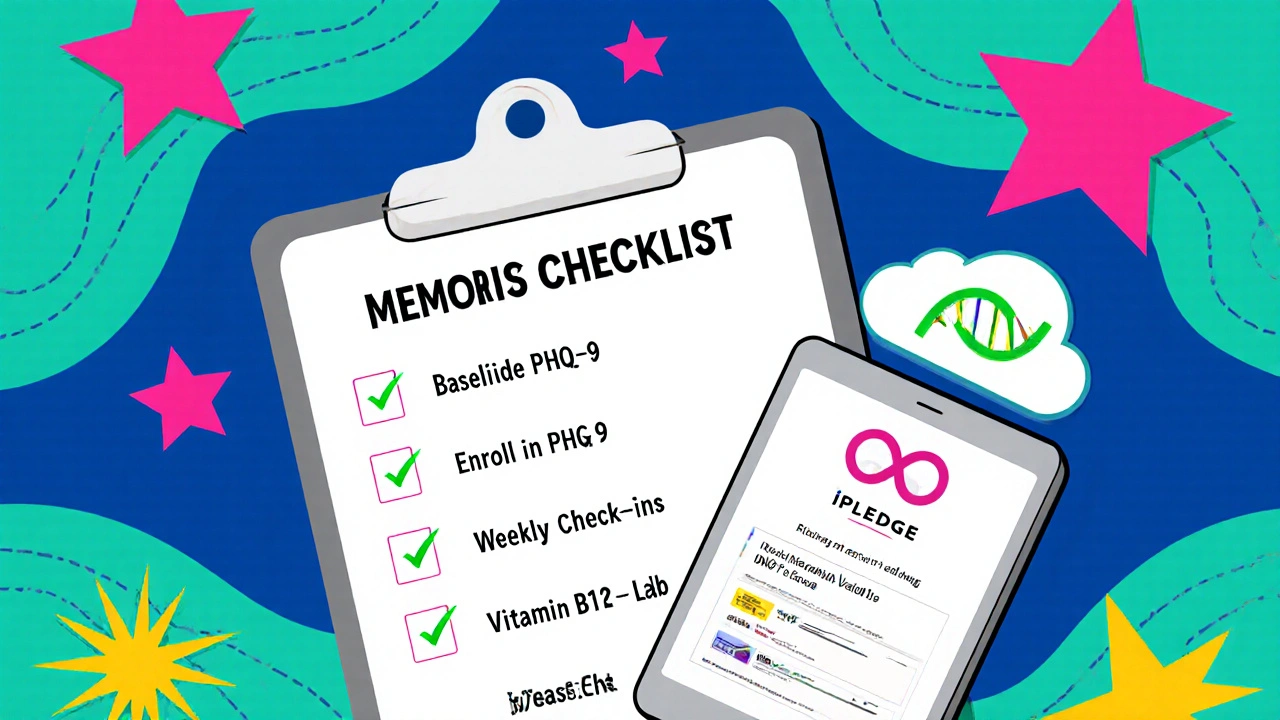
Practical Checklist for Clinicians
- Document baseline psychiatric history and PHQ‑9 score.
- Enroll the patient in iPLEDGE and complete the required mental‑health training.
- Schedule weekly check‑ins for the first month, then follow the monitoring timeline.
- Use the PHQ‑9 threshold (≥10) as a trigger for immediate psychiatric referral.
- Educate patients on red‑flag symptoms and encourage honest reporting.
- If red flags arise, pause isotretinoin, arrange urgent mental‑health evaluation, and discuss alternatives.
- Record all assessments in the EMR, noting any vitamin B12 labs if mood changes occur.
Common Patient Questions Answered
Will isotretinoin make me depressed?
Most people don’t develop depression on isotretinoin. Studies show the absolute risk is similar to the general population, but the drug does raise the relative reporting of mood changes. That’s why regular screening is essential.
How soon after starting treatment should I expect mood changes?
The median onset is about 80 days, with many reports appearing in the first eight weeks. Weekly check‑ins during that period help catch issues early.
What screening tool is used?
The Patient Health Questionnaire‑9 (PHQ‑9) is the standard in the U.S. and many other countries. Some clinics also use the Beck Depression Inventory for a second opinion.
If I develop depression, can I continue the medication?
Mild, manageable symptoms can be treated alongside isotretinoin, but any moderate‑to‑severe depression, suicidal thoughts, or rapid mood swings should prompt a pause and psychiatric referral.
Are there any lab tests I need?
Baseline liver function tests and lipid panels are routine. If mood changes occur, checking vitamin B12 levels is recommended because deficiency can mimic depression.
By weaving together the latest data, regulatory expectations, and practical clinic workflows, you can prescribe isotretinoin with confidence while safeguarding your patients’ mental well‑being.


8 Comments
Tim Waghorn
October 26, 2025 AT 14:21When prescribing isotretinoin, a clinician must first establish a baseline mental‑health profile to distinguish drug‑related mood changes from pre‑existing conditions.
The PHQ‑9 score at baseline provides a quantifiable metric that can be tracked over the treatment course.
A score of less than five generally indicates minimal depressive symptoms, whereas a score of ten or higher warrants closer observation.
Given that the median onset of psychiatric symptoms occurs around eighty days, weekly check‑ins during the first month become essential.
These check‑ins can be conducted via secure messaging platforms, allowing patients to report subtle mood shifts without the stigma of an in‑person visit.
If a patient’s PHQ‑9 increases by five points between assessments, the clinician should consider a temporary pause of isotretinoin pending psychiatric evaluation.
The iPLEDGE program now integrates digital PHQ‑9 submissions, automatically flagging scores above the threshold for immediate review.
In addition to questionnaire data, clinicians should monitor for red‑flag behaviors such as expressions of hopelessness, sudden irritability, or withdrawal from daily activities.
While vitamin B12 deficiency can mimic depressive symptoms, a simple serum test can rule out this confounding factor before attributing mood changes to the retinoid.
Patients with a documented history of bipolar disorder may require more frequent assessments, perhaps bi‑weekly, to capture rapid mood cycling.
It is also advisable to coordinate care with a mental‑health professional who can provide psychotherapy or pharmacologic support if needed.
Should severe depression or suicidal ideation arise, isotretinoin must be discontinued and an urgent psychiatric referral initiated.
Alternative acne treatments, such as doxycycline or topical retinoids, can be employed while the patient receives mental‑health care.
Documentation of each assessment in the electronic medical record ensures compliance with regulatory requirements and provides medicolegal protection.
By adhering to this structured monitoring protocol, clinicians can minimize psychiatric risk while preserving the therapeutic benefits of isotretinoin.
Brady Johnson
November 7, 2025 AT 04:10Your checklist reads like a bureaucratic nightmare, but the truth is that most patients never notice any mood dip.
The data you cite are cherry‑picked from databases that love to scream for attention.
In practice, I’ve seen far fewer crises than your alarmist tone suggests.
If you keep inflating the risk, you’ll scare away people who desperately need the drug.
Bottom line: monitor, but don’t turn every acne patient into a psychiatric case.
Laura Hibbard
November 18, 2025 AT 18:13Wow, so the answer to ‘Will isotretinoin make me depressed?’ is basically ‘maybe, but probably not.’
I guess the universe loves to give us vague reassurance wrapped in statistics.
Sounds like a perfect compromise for anyone who loves paperwork.
At least we have a schedule to fill our calendars.
Rachel Zack
November 30, 2025 AT 08:16Honestly, treating teens like lab rats is just wrong its a violation of trust.
Doctors should put patients first not worry about tick boxes.
If you push meds without real consent it feels like exploitation.
Lori Brown
December 11, 2025 AT 22:20Great guide-feeling more confident about monitoring now 😊
Jennyfer Collin
December 23, 2025 AT 12:23While the recommendation appears evidence‑based, one must consider the possibility that pharmaceutical sponsors influence the monitoring thresholds 😐.
Carla Smalls
January 4, 2026 AT 02:26Remember, you’re not alone in this; having a mental‑health partner alongside your dermatologist can make the process much smoother.
Megan Dicochea
January 15, 2026 AT 16:30That's true.
It helps a lot.
Keep the schedule simple.