Imagine taking a pill that could save your life - but only if you get the exact right dose. Too little, and it doesn’t work. Too much, and it could land you in the hospital. That’s the reality for people taking narrow therapeutic index drugs - or NTI drugs. These aren’t your average medications. They’re like walking a tightrope. One wrong step, and things can go wrong fast.
What Exactly Are NTI Drugs?
NTI drugs have a tiny window between being effective and being dangerous. The difference between the dose that helps you and the dose that harms you is so small, even a 10% change in your blood level can cause serious problems. The U.S. Food and Drug Administration (FDA) defines them as medications where even small changes in dose or blood concentration can lead to life-threatening side effects or treatment failure.
Think of it like a thermostat. If your home’s ideal temperature is 72°F, and anything below 70°F makes you shiver or above 74°F makes you sweat, that’s a narrow range. NTI drugs work the same way. The body doesn’t have much room to spare.
These drugs are not rare. About 5-7% of all prescription medications fall into this category - but they’re responsible for nearly 15% of all serious drug-related hospitalizations. That’s because even tiny changes in how your body absorbs or processes them can have big consequences.
Common NTI Drugs You Might Be Taking
You might already be on one of these without realizing it. Here are some of the most common NTI drugs:
- Warfarin (Coumadin, Jantoven): Used to prevent blood clots. Too low, and you risk stroke or clotting. Too high, and you could bleed internally.
- Lithium (Lithobid): Helps manage bipolar disorder. Levels above 1.5 mmol/L can cause tremors, confusion, or seizures.
- Levothyroxine (Synthroid): Replaces thyroid hormone. Even small changes in dose can make you feel exhausted, gain weight, or have heart palpitations.
- Digoxin (Lanoxin): Treats heart failure and irregular heartbeat. Toxic levels can trigger dangerous heart rhythms.
- Tacrolimus (Prograf): Used after organ transplants to prevent rejection. Too low? Your body attacks the new organ. Too high? Your kidneys get damaged.
- Phenytoin (Dilantin) and Carbamazepine (Tegretol): Used for seizures. Small changes can cause seizures to return or lead to dizziness, nausea, or even coma.
- Methotrexate (Trexall): Used for autoimmune diseases and some cancers. Overdose can damage your liver and bone marrow.
Each of these requires regular blood tests to make sure you’re in the safe zone. For example, warfarin patients need INR tests every 1-4 weeks. Lithium levels are checked every 3-6 months - more often if your dose changes.
Why Generic Substitutions Can Be Risky
One of the biggest risks with NTI drugs is switching between brand-name and generic versions - or even between different generic brands.
Most generic drugs are considered interchangeable with their brand-name counterparts. But for NTI drugs, that’s not always true. Even small differences in how the pill is made - like the filler ingredients or how quickly it dissolves - can change how much of the drug enters your bloodstream.
A patient taking levothyroxine switched from one generic brand to another and saw their TSH level jump from 1.8 to 8.4 in just six weeks. That’s a massive shift. They went from feeling fine to exhausted, gaining weight, and struggling to concentrate.
In another case, a warfarin user switched to a generic version and saw their INR spike from 2.5 to 4.1 in a week - a level that puts you at high risk for internal bleeding. They needed emergency treatment with vitamin K.
The FDA and European Medicines Agency (EMA) have responded by tightening standards. For NTI drugs, generic manufacturers must prove their product stays within a 90-111% range of the brand-name drug’s absorption - much tighter than the standard 80-125% used for most generics.
Some states, like North Carolina, require pharmacists to get your doctor’s approval before switching your NTI drug to a generic. That’s because the risk isn’t theoretical - it’s happened to real people.
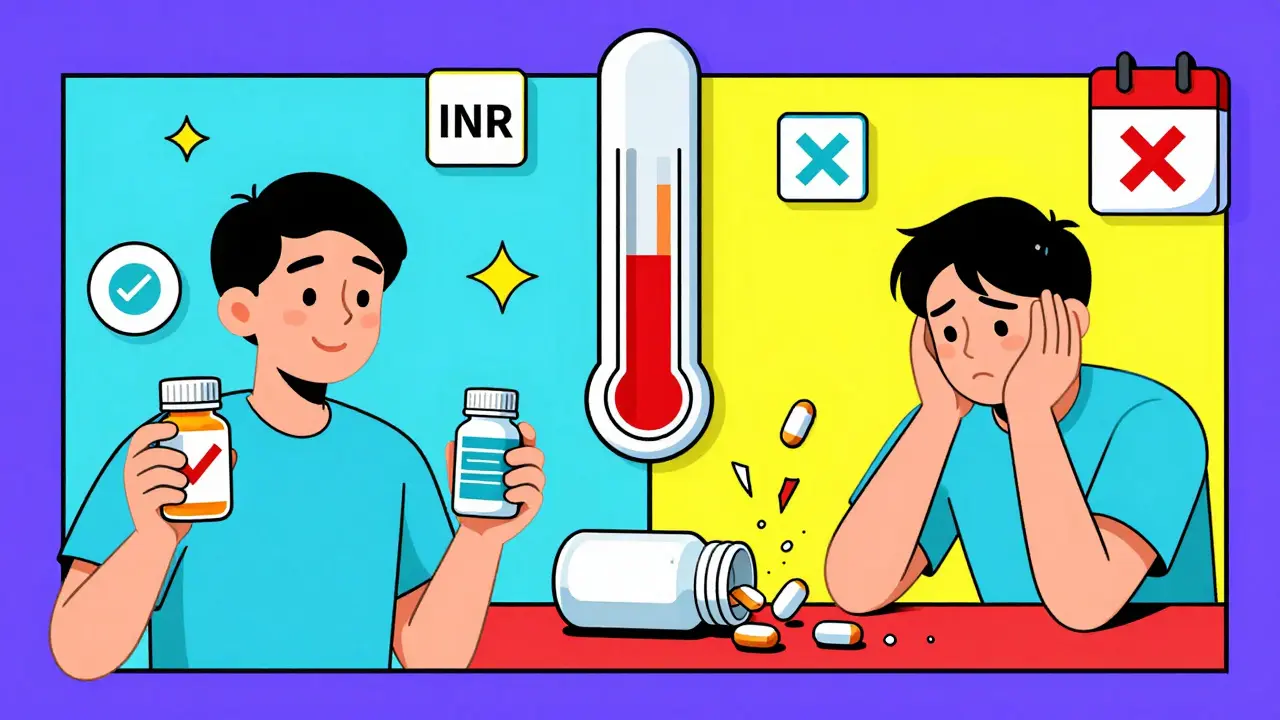
Monitoring: Your Lifeline
If you’re on an NTI drug, regular blood tests aren’t optional. They’re essential. These tests tell your doctor whether the drug is working at the right level in your body.
Here’s what monitoring typically looks like:
- Warfarin: INR test every 1-4 weeks (or more often if your dose changes)
- Lithium: Blood level every 3-6 months; more often after starting or changing dose
- Digoxin: Blood level every 6-12 months, or if you feel dizzy or nauseous
- Tacrolimus: Twice a week after transplant, then weekly or monthly as you stabilize
- Levothyroxine: TSH and free T4 every 6-8 weeks after starting, then every 6-12 months if stable
Many patients say the hardest part isn’t the blood draws - it’s remembering to go. One Reddit user with bipolar disorder shared that consistent lithium monitoring kept them out of the hospital for 8 years. Before that, they had three hospitalizations in two years.
Keep a log. Write down your test results, how you’re feeling, and any changes in your routine. This helps your doctor spot trends early. Studies show patients who track their symptoms and lab values have 32% fewer adverse events.
What You Can Do to Stay Safe
Managing an NTI drug isn’t just about taking pills. It’s about building habits that protect you.
- Stick to one pharmacy. If you switch pharmacies, you might get a different generic version. Keep your prescriptions at one place so they know your history.
- Never switch generics without talking to your doctor. Even if the label says “equivalent,” ask: “Is this safe for my NTI drug?”
- Know the warning signs. For warfarin: unusual bruising, nosebleeds, dark urine. For lithium: hand tremors, confusion, vomiting. For levothyroxine: rapid heartbeat, weight loss, or extreme fatigue.
- Watch your diet and other meds. Warfarin interacts with vitamin K-rich foods (like spinach and kale). Lithium is affected by salt intake and NSAIDs like ibuprofen. Always tell your doctor about every supplement or over-the-counter drug you take.
- Use reminders. Set phone alarms for blood tests and pill times. Missing a dose or a test can be dangerous.
The Future of NTI Drug Safety
Things are getting better. The FDA is working on a formal list of NTI drugs with clear rules for testing and switching. They’ve also approved apps that help patients track doses, symptoms, and lab results.
Researchers are now studying how your genes affect how you respond to these drugs. For example, some people have genetic variants that make them process warfarin much slower. These patients need much lower doses. By 2026, genetic testing before starting certain NTI drugs may become standard - and could cut adverse events by up to 35%.
Hospitals are also using barcode scanning for high-risk NTI drugs to prevent dosing errors. If a nurse scans your wristband and the drug, the system checks if the dose matches your profile. It’s a small step - but it saves lives.
You’re Not Alone
Living with an NTI drug can feel overwhelming. But you’re not the only one managing this. Millions of people take these medications and live full, stable lives - because they stay informed and stay involved.
It’s not about being perfect. It’s about being consistent. Show up for your tests. Ask questions. Speak up if you feel off. Your doctor needs you as a partner in your care.
NTI drugs aren’t scary when you understand them. They’re powerful tools - but they demand respect. Treat them with care, and they’ll treat you well.
Are all generic drugs unsafe for NTI medications?
No, not all generics are unsafe. But for NTI drugs, even small differences between brands can matter. Some generic versions work just fine, but switching between them without monitoring can be risky. Always check with your doctor before switching, and never accept a different generic without knowing if it’s been tested for your specific drug.
How often do I need blood tests for NTI drugs?
It depends on the drug and your situation. For warfarin, expect tests every 1-4 weeks. For lithium, every 3-6 months when stable, but more often when starting or changing dose. Tacrolimus requires frequent checks early after transplant - sometimes twice a week. Your doctor will adjust the schedule based on your stability and response.
Can I switch from brand to generic or vice versa?
Only under your doctor’s supervision. Even if the pharmacy says they’re the same, NTI drugs aren’t interchangeable like other medications. A switch can cause your blood levels to change, leading to side effects or treatment failure. Always get your doctor’s approval before changing.
What should I do if I miss a dose?
Don’t double up. Call your doctor or pharmacist immediately. For drugs like warfarin or lithium, missing a dose can affect your levels for days. Your provider will tell you whether to skip it, take it late, or adjust your next dose - based on your specific drug and situation.
Can diet or other medications affect my NTI drug?
Yes, very much so. Warfarin interacts with vitamin K (found in leafy greens), alcohol, and some antibiotics. Lithium is affected by salt, dehydration, and NSAIDs like ibuprofen. Levothyroxine should be taken on an empty stomach - food, coffee, calcium, or iron supplements can block absorption. Always tell your doctor about everything you take - even supplements and herbal products.
Is there a list of all NTI drugs?
The FDA doesn’t publish an official public list, but they recognize certain drugs as NTI based on expert consensus and clinical data. Common ones include warfarin, lithium, levothyroxine, digoxin, tacrolimus, phenytoin, and methotrexate. If your doctor says your drug is an NTI drug, treat it as one - regardless of whether it’s on a list.


15 Comments
Sahil jassy
December 19, 2025 AT 17:06Been on warfarin for 5 years 🙌 Just stick to one pharmacy and get your INR checked. No drama, no switches. Life’s easier that way.
Chris Clark
December 21, 2025 AT 05:21I work in a pharmacy in Texas and let me tell ya, we get so many people switching generics for levothyroxine and then showing up with TSH levels off the charts. It’s wild. Docs need to be louder about this. Not all generics are created equal, especially for NTI drugs.
Nina Stacey
December 22, 2025 AT 21:13I was on lithium for years and honestly the hardest part wasn't the meds it was remembering to get blood drawn every 3 months I'd forget and then feel like a zombie for weeks until I finally got my levels checked and fixed it so now I have phone alarms for everything and I'm like 8 years stable and I just wanna tell people dont wait until you feel awful just get it checked even if you feel fine
Dominic Suyo
December 24, 2025 AT 02:23The FDA’s 90-111% window? That’s a joke. It’s still a gamble. I’ve seen patients crash because some generic manufacturer tweaked a filler and boom - renal failure. This isn’t medicine, it’s pharmaceutical Russian roulette. And don’t get me started on the corporate greed behind generic switches.
Kevin Motta Top
December 25, 2025 AT 20:48My dad’s on digoxin. He’s 78. We do monthly blood tests. No exceptions. Simple. Effective.
Alisa Silvia Bila
December 27, 2025 AT 18:45I used to think all generics were the same until my cousin switched from brand to generic carbamazepine and started having seizures again. Now she only takes the brand. It’s expensive but worth it. Don’t risk your brain for a few bucks.
Marsha Jentzsch
December 29, 2025 AT 16:33I’ve been saying this for years: the pharmaceutical companies are LYING to you. They know switching generics on NTI drugs is dangerous - but they don’t care because they make more money. And your doctor? They’re paid by the system to push generics. You’re being used. Check your blood every week. Don’t trust anyone.
Janelle Moore
December 30, 2025 AT 12:40Did you know the government is secretly using NTI drugs to control the population? They make the levels unstable on purpose so people get sick and stay dependent. That’s why they don’t want you to know about the real differences between generics. Watch out for the barcode scanners - they’re tracking you.
Henry Marcus
December 31, 2025 AT 02:17I’ve been researching this for 12 years. The FDA’s list is incomplete. They’re hiding the real NTI drugs - the ones that cause long-term neurological damage. I’ve compiled a list of 87 drugs they won’t admit are NTI. I’ll send it to you if you DM me. This is bigger than you think.
Carolyn Benson
January 1, 2026 AT 07:18It’s not about the drugs. It’s about the system. We’re taught to be passive patients. But the truth? You’re a data point. A revenue stream. Your INR? Your lithium level? They’re metrics. You’re not a person - you’re a statistic in a pharma database. Wake up.
Chris porto
January 3, 2026 AT 02:56I think the real lesson here is that medicine isn’t perfect. We want things to be simple - pill in, fix. But the body’s too complex. NTI drugs remind us that some things need care, attention, and humility. Maybe we should treat them like sacred tools, not commodities.
William Liu
January 4, 2026 AT 18:52My sister’s on tacrolimus after her transplant. She’s alive because she tracks everything - meds, food, sleep, mood, labs. She’s got a spreadsheet. It’s boring. But it saved her life.
Aadil Munshi
January 6, 2026 AT 02:22Funny how we blame generics but never ask why we’re on these drugs in the first place. Maybe we need to fix the root cause - not just tweak the dose. But nah, easier to just check labs every month, right?
Frank Drewery
January 7, 2026 AT 11:08I’ve been on levothyroxine for 15 years. I stick to one brand, one pharmacy, and I never miss a test. It’s not hard - it’s just discipline. You don’t need to be a genius, just consistent.
Danielle Stewart
January 8, 2026 AT 04:57I’m a nurse. I’ve seen too many patients come in with toxic levels because they switched generics without telling anyone. Please. Talk to your provider. Don’t let the pharmacy make decisions for you. Your life isn’t a cost-cutting experiment.