Why Your Family Needs an Overdose Emergency Plan
Every year, over 100,000 people in the U.S. die from drug overdoses. Most of those deaths involve opioids - especially synthetic ones like fentanyl - and many happen at home. The scary part? You don’t need to be a drug user to be at risk. If someone in your household takes prescription painkillers, even just occasionally, you’re one unexpected mistake or accidental mix away from a crisis.
Here’s the truth: 93% of opioid overdoses can be reversed if naloxone is given within minutes. But only 12% of families with prescription opioids have a plan. That means 88% of households are flying blind. This isn’t about fear. It’s about preparation. Think of it like a fire extinguisher. You hope you never need it. But if you do, you want it right there, you know how to use it, and everyone else in the house does too.
Step 1: Know Who’s at Risk
Not every household needs this plan. But if any of these apply to someone living with you, you need one now:
- They take opioid pain meds like oxycodone, hydrocodone, morphine, or fentanyl patches
- They’ve been on opioids for more than a few weeks
- They take more than one medication that affects the brain - like benzodiazepines (Xanax, Valium), sleep aids, or alcohol
- They’ve had a past overdose, even if it was years ago
- They’ve struggled with addiction or mental health issues
- They’re over 65 - older adults are more sensitive to opioids
According to CDC data, over 51 million U.S. adults got opioid prescriptions in 2022. That’s not a small number. If your mom takes oxycodone for back pain, your teen takes Adderall and drinks alcohol, or your dad uses fentanyl patches after surgery - you’re not immune. You’re just unprepared.
Step 2: Get Naloxone - And Keep It Accessible
Naloxone is the only medicine that can reverse an opioid overdose. It’s safe, non-addictive, and works in minutes. You can get it without a prescription in 46 states, including all of Australia’s neighboring regions. In the U.S., most pharmacies - CVS, Walgreens, Rite Aid - offer it for $25 or less with insurance. Many even give it away for free.
Don’t store it in the medicine cabinet. Don’t lock it up. Don’t keep it in the car. Keep it where you keep your phone - on the kitchen counter, in a drawer by the front door, in your partner’s purse. The goal is speed. Every second counts.
Buy two or three doses. Fentanyl is so strong, one dose of naloxone might not be enough. The Washington State Department of Health recommends keeping at least two doses on hand. Check the expiration date every 18 months. Naloxone doesn’t go bad overnight, but it loses effectiveness over time. Replace it before it expires.
Step 3: Learn the Signs of an Overdose
An overdose doesn’t always look like what you see on TV. People don’t always collapse dramatically. Often, they’re just… still. Here’s what to look for:
- Unresponsive: Shake their shoulder hard. Yell their name. If they don’t wake up, it’s not sleep - it’s overdose.
- Slow or no breathing: Count their breaths for 15 seconds. If they take fewer than four breaths, they’re in danger. Their lips or fingernails may turn blue or gray.
- Pinpoint pupils: Shine a light in their eye. If the black center is tiny like a pinprick, that’s a classic sign.
Don’t wait for all three. If two are present - especially unresponsiveness and slow breathing - act immediately. Fentanyl can knock someone out in under three minutes. Waiting even a minute can be fatal.
Step 4: Practice the Response - Every Time
There’s no time to read instructions when someone’s not breathing. You need to know what to do without thinking. Here’s the simple six-step plan, based on the A.N.C.H.O.R. method used by New York’s Project COPE:
- Assess: Check for unresponsiveness and slow breathing. Don’t waste time looking for pills or bottles.
- Naloxone: Administer one dose of naloxone nasal spray (Narcan) into one nostril. If you’re using the injection, give it into the thigh muscle. No need to undress them - just push through clothing.
- Call 911: Do this right after giving naloxone. Say: “Someone is unresponsive and not breathing. We’ve given naloxone.”
- Have more ready: Keep the second dose in your hand. If they don’t wake up in 3-5 minutes, give another dose.
- Observe: Stay with them. Even if they wake up, they can crash again in the next 2-4 hours. This is called renarcotization. Don’t let them go back to sleep.
- Review: After the crisis, talk as a family. What worked? What didn’t? Update your plan.
Practice this once a month. Just 10 minutes. One person plays the overdosing person, another does the steps. It builds muscle memory. The American Red Cross found that families who practiced monthly retained 89% of their skills after three months. Those who didn’t? Only 32% remembered correctly.
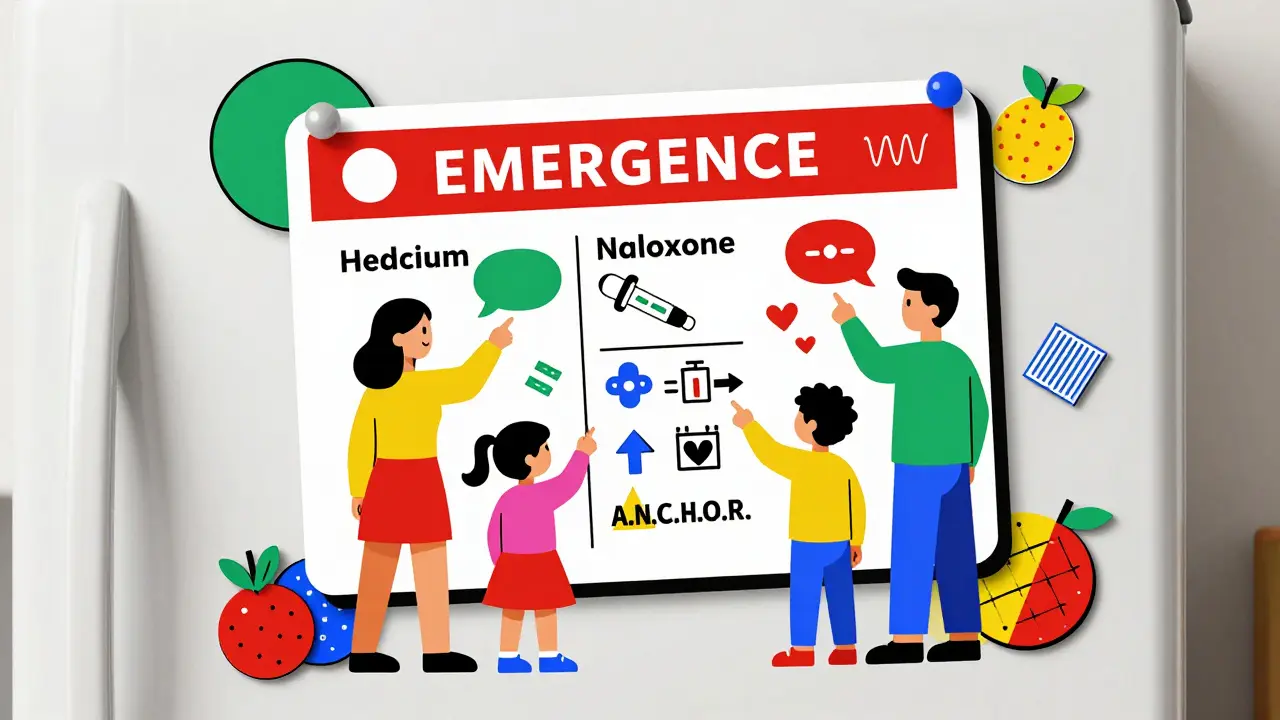
Step 5: Make a Simple, Visible Emergency Card
What if your teenager finds their dad unconscious and you’re not home? What if your elderly parent can’t remember what to do?
Create a laminated card. Put it on the fridge. Give one to each adult in the house. Include:
- Names of all household members on opioids
- Medication names and doses
- Doctor’s name and phone number
- Where the naloxone is stored
- Emergency contacts (911, poison control, a neighbor who knows the plan)
- Simple step-by-step instructions (like the A.N.C.H.O.R. steps above)
Ohio’s 2022 trial showed this reduced response time by nearly 50 seconds. In an overdose, that’s the difference between life and death.
Step 6: Talk About It - Even When It’s Hard
The biggest barrier isn’t cost or access. It’s silence. Families avoid talking about overdose because it feels like inviting disaster. But avoiding the conversation is riskier.
Start small. Say: “I read that naloxone can save lives. I think we should have one in the house, just in case.” Don’t make it about addiction. Make it about safety. Like seatbelts. Like smoke alarms.
Teach your kids. The 2023 National Youth Risk Behavior Survey found 34% of teens aged 14-17 know someone who’s overdosed. They might be the first to find someone unresponsive. They need to know what to do - and that it’s okay to call 911 without fear.
Good Samaritan laws protect anyone who calls for help. In all 50 states, you can’t be arrested for giving naloxone or calling 911 during an overdose. That’s not a rumor. That’s the law.
What This Plan Won’t Fix
This plan saves lives during an overdose. It doesn’t cure addiction. It doesn’t replace treatment. But here’s the good news: 89% of people who survive an overdose with naloxone go on to seek help. That’s not coincidence. It’s hope.
Some experts worry that having naloxone gives people a false sense of security. But the data says otherwise. Naloxone doesn’t encourage use. It gives people a second chance. And that second chance? It’s often the start of recovery.
Resources You Can Use Right Now
- Free naloxone: Visit your local pharmacy. Ask for it. No prescription needed in most places.
- Free training: The American Red Cross offers a free 15-minute online course. Search “Red Cross Overdose Response” - it takes less time than scrolling Instagram.
- Emergency apps: The “Overdose Guardian” app (released Jan 2024) sends alerts if overdose calls spike in your ZIP code. It’s free and works offline.
- Insurance: Under the 2024 Inflation Reduction Act, Medicare Part D covers naloxone with $0 copay. Private insurers? 41% still charge $25-$50. Call your plan. Ask for a waiver.
Final Thought: This Isn’t About Fear. It’s About Love.
You don’t make a plan because you expect the worst. You make it because you love someone enough to be ready for it. You don’t need to be a doctor. You don’t need to be brave. You just need to be prepared.
Right now, someone in your home might be taking a medication that could kill them if mixed wrong. Or if they take one too many. Or if they accidentally take someone else’s pill.
That person isn’t a statistic. They’re your parent. Your child. Your partner. Your sibling.
Make the plan. Buy the naloxone. Practice the steps. Talk about it.
Because when the moment comes - and you don’t know if it will - you’ll be ready. And that’s the most powerful thing you can do.


4 Comments
Carolyn Whitehead
January 29, 2026 AT 23:17I just bought two Narcan kits after reading this. Put one by the coffee maker and one in my partner’s purse. No more pretending this won’t happen to us.
It’s weird how something so simple can feel so heavy.
Gaurav Meena
January 31, 2026 AT 14:57This is life-saving stuff 😊 I shared it with my whole family back in India-even my aunt who takes painkillers after her knee surgery. We’re getting naloxone next week. No shame in being prepared!
Jodi Olson
February 2, 2026 AT 14:00The framing of this as an act of love rather than fear is profoundly correct. Preparedness is not morbid it is the quietest form of care we can offer another human being
Marc Bains
February 3, 2026 AT 19:01I teach this to my college students every semester. They think it’s dystopian until they realize their roommate’s cousin OD’d last year. Then they get it. Knowledge is the first dose of hope.