By the time you turn 65, there’s a one in three chance you’re already struggling to hear conversations clearly - not because you’re not paying attention, but because your ears have changed. This isn’t just about turning up the TV. It’s presbycusis, the medical term for age-related hearing loss, and it’s quietly reshaping how millions of older adults connect with the world.
What Exactly Is Presbycusis?
Presbycusis (pronounced prez-buh-KYOO-sis) isn’t just "getting a little deaf." It’s a gradual, permanent loss of hearing caused by changes inside the inner ear. Specifically, the tiny hair cells in your cochlea - the ones that turn sound waves into electrical signals your brain understands - start dying off. You’re born with about 16,000 of them. And once they’re gone, they don’t come back.
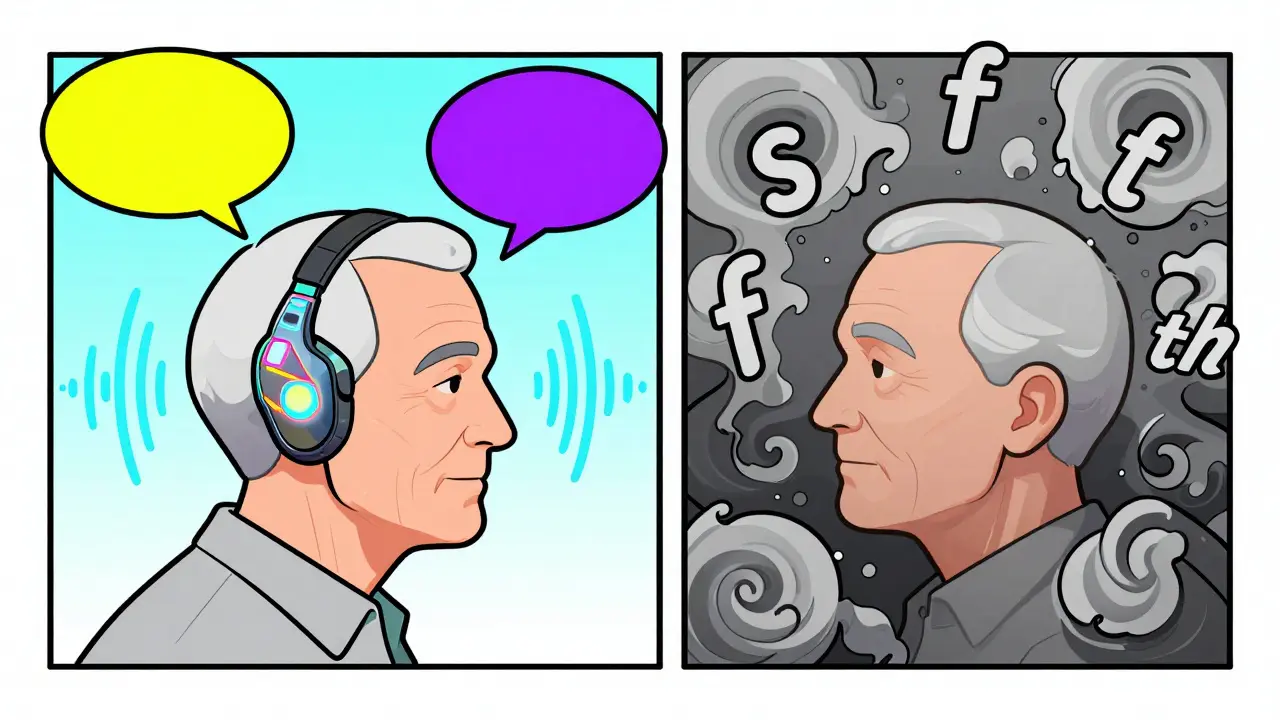
This isn’t sudden. It creeps in over years. At first, you might not even notice. But then you start asking people to repeat themselves. You find yourself nodding along in group chats because you can’t pick out individual voices. High-pitched sounds - like children’s voices, birds chirping, or the beeping of a microwave - become fuzzy or disappear entirely. Consonants like "s," "th," and "f" blend together, making speech sound muffled even when it’s loud enough.
By age 75, nearly half of all adults have significant hearing loss. The National Institute on Deafness and Other Communication Disorders (NIDCD) reports that 37.5 million Americans over 18 already deal with some level of hearing difficulty. And it’s not just about missing words - it’s about missing life.
Why Does This Happen?
It’s not just aging. While the natural breakdown of hair cells is the main driver (responsible for about 65% of cases), other factors speed things up. Genetics play a big role - if your parents or grandparents had trouble hearing later in life, you’re more likely to too. Genes like GRHL2 and GJB2 have been linked to this vulnerability.
Environmental damage adds up. If you worked in a noisy factory, went to loud concerts without protection, or spent years using headphones at high volume, you’ve already lost ground. Exposure to sounds over 85 decibels for more than eight hours a day increases your risk of presbycusis by 40%.
Health conditions also chip away at your hearing. Diabetes raises your risk by 28%. High blood pressure by 23%. Even smoking increases it by 15%. These conditions reduce blood flow to the inner ear, starving the hair cells of oxygen. Medications like certain antibiotics or high-dose aspirin can also contribute, though this is less common.
It’s a perfect storm: time, genes, noise, and health all team up to quietly steal your hearing. And the worst part? Most people don’t realize how much they’ve lost until it’s already affecting their relationships, safety, and mental health.
The Hidden Costs of Untreated Hearing Loss
People often think, "I can just lip-read" or "I’ll turn up the volume." But the damage goes far beyond missed conversations.
Studies show untreated hearing loss increases your risk of dementia by up to 50%. Why? Because your brain has to work harder to decode sounds, draining energy that should go to memory and thinking. A 2020 Lancet Commission report found that treating hearing loss could be one of the most effective ways to reduce dementia risk - even more than quitting smoking or exercising regularly.
Then there’s isolation. People with hearing loss are 5.3 times more likely to withdraw from social events. Forty-one percent avoid gatherings because they’re tired of pretending they heard everything. Twenty-nine percent report missing important medical instructions during doctor visits. That’s not just inconvenient - it’s dangerous.
Depression rates jump by 32% in those with unaddressed hearing loss. And financially, the impact is real. A 2021 study found people with untreated hearing loss earn $30,000 less per year on average than their peers with normal hearing - not because they’re less capable, but because communication gaps limit career growth and confidence.
And safety? Thirty-seven percent of older adults with hearing loss have missed a fire alarm, car horn, or doorbell at least once in the past year. That’s not a minor inconvenience - it’s a life-or-death risk.
Amplification Isn’t Just a Device - It’s a Lifeline
The good news? Hearing loss doesn’t have to mean silence. Amplification strategies - primarily hearing aids - can restore connection. Modern devices aren’t just speakers that make everything louder. They’re tiny computers that listen, analyze, and adjust in real time.
Today’s hearing aids use 16 to 64 frequency channels to boost only the sounds you need to hear - like speech - while suppressing background noise. Directional microphones improve your ability to focus on someone talking to you in a restaurant by 3 to 6 decibels. Bluetooth lets you stream calls, music, and TV audio directly to your ears. Some even track your steps, heart rate, or how often you’re engaging socially.
Properly fitted hearing aids can improve speech understanding by 40-60% in quiet settings and 25-40% in noisy ones. Eighty-five percent of users report better communication after getting them. But here’s the catch: only 30% of people who could benefit actually use them.
Why? Cost is a big barrier. Prescription hearing aids range from $1,800 to $3,500 per ear. Many people assume they’re out of reach. But since the FDA legalized over-the-counter (OTC) hearing aids in 2022, options under $1,000 have exploded. Brands like Jabra Enhance Select and Eargo offer solid performance at a fraction of the price.
And help is getting more accessible. Medicare Advantage plans now cover hearing aids for over 28 million beneficiaries. Telehealth audiology services let you get your device fine-tuned from home. Many clinics offer 30- to 60-day trials so you can test-drive a device before committing.
What Works Best? Top Models and Real-World Feedback
Not all hearing aids are created equal. Based on 2023 Consumer Reports ratings, the top prescription models are Widex Moment (87/100) and Oticon More (85/100). Both use advanced AI to reduce listening effort and adapt to changing environments. For OTC, Jabra Enhance Select leads at 78/100, praised for its easy app control and comfort.
But user experience matters more than specs. On Reddit’s r/HearingAids community, people share stories like this: "After 15 years of pretending to hear, my Phonak Audeo M-312s restored my ability to hear my granddaughter’s laughter clearly." That’s the kind of moment amplification makes possible.
Still, challenges remain. Thirty-eight percent of users struggle with wind noise. Twenty-seven percent have Bluetooth connection issues. Forty-two percent say restaurants are still too hard to navigate - even with hearing aids. And 20% quit using their devices within six months. Why? Poor fit (45%), discomfort (30%), or disappointment that it doesn’t "fix" hearing completely (25%).
Realistic expectations are key. Hearing aids don’t restore your hearing to what it was at 25. They make communication easier. Most users reach 80% comfort within 4 to 6 weeks. But learning to use features like smartphone apps takes about 12 hours of practice.

Getting Started: What to Do Now
If you suspect you have presbycusis, don’t wait. The American Speech-Language-Hearing Association (ASHA) recommends a baseline hearing test at age 50, then every two years. Early detection means better outcomes. Treating hearing loss at 60 instead of 70 could reduce your dementia risk by 8-10% over a decade, says Dr. Frank R. Lin from Johns Hopkins.
Start with a licensed audiologist. They’ll test your hearing, rule out other causes (like earwax buildup or infections), and recommend the right device. Avoid online-only sellers who don’t offer follow-up support. A good fit matters more than price.
Ask about:
- A 30- to 60-day trial period
- Follow-up appointments for adjustments
- Rechargeable vs. battery-powered models
- Bluetooth and app compatibility
- Warranty and repair options
Don’t be afraid to try more than one model. What works for your neighbor might not work for you. Your ear shape, lifestyle, and budget all matter.
The Bigger Picture
The global hearing aid market is projected to hit $14.7 billion by 2030. Why? Because the numbers are rising fast. The World Health Organization predicts 1.5 billion people will have hearing loss by 2050 - triple today’s number. That’s not just a health issue. It’s a public health emergency.
But here’s the hopeful part: we have the tools to fix this. Hearing aids work. They’re more advanced, affordable, and accessible than ever. The barrier isn’t technology - it’s awareness. Only 15% of primary care doctors routinely screen for hearing loss, even though it’s recommended.
If you’re over 50, get tested. If you’re helping an older parent or grandparent, encourage them to take the first step. Hearing loss doesn’t have to mean loneliness, danger, or decline. With the right amplification, connection is still possible - even at 80, 90, or beyond.
Is presbycusis the same as general hearing loss?
No. Presbycusis is a specific type of hearing loss caused by aging, primarily affecting the inner ear’s hair cells. Other types of hearing loss can be caused by noise exposure, infections, head injuries, or medications. Presbycusis is progressive, sensorineural, and happens naturally over time.
Can hearing aids restore my hearing to normal?
No, they can’t restore your hearing to what it was when you were younger. But they can significantly improve your ability to understand speech, especially in noisy environments. Most users report 40-60% improvement in quiet settings and 25-40% in noisy ones. The goal isn’t perfection - it’s connection.
Are over-the-counter (OTC) hearing aids any good?
Yes - for mild to moderate hearing loss. Since the FDA approved OTC hearing aids in 2022, models like Jabra Enhance Select and Eargo have become popular for their affordability and ease of use. They’re not ideal for severe loss or complex needs, but for many, they’re a great first step. Always get a hearing test first to confirm your type of loss.
Why do some people stop using hearing aids?
The top reasons are poor fit (45%), discomfort (30%), and not hearing well in noisy places like restaurants (25%). Many users expect immediate perfection. But adaptation takes time - typically 4 to 6 weeks. Working with an audiologist for adjustments during the first few months dramatically improves success rates.
Does Medicare cover hearing aids?
Original Medicare (Parts A and B) does not cover hearing aids. But many Medicare Advantage plans (Part C) now do. As of 2024, over 28 million beneficiaries have coverage through these plans. Check your specific plan’s benefits - coverage varies by provider and region.
How often should I get my hearing checked after 50?
The American Speech-Language-Hearing Association recommends a baseline test at age 50, then every two years. If you notice changes - like struggling in crowds, turning up the TV, or hearing ringing in your ears - get tested sooner. Early detection leads to better outcomes and helps preserve your brain’s ability to process sound.
Can hearing loss lead to dementia?
Yes, untreated hearing loss is linked to a 50% increased risk of dementia. When your brain struggles to process sound, it overworks other areas, draining energy needed for memory and thinking. Studies show treating hearing loss early - especially by age 60 - can reduce dementia risk by 8-10% over ten years.
What’s Next?
If you’ve been putting off a hearing test because you think it’s "just part of getting older," reconsider. This isn’t about vanity - it’s about staying safe, connected, and independent. The tools exist. The science is clear. The only thing left is taking action.
Start with a simple step: schedule a hearing screening. It’s quick, painless, and often free through local clinics or pharmacies. Don’t wait for a crisis. The sooner you act, the more of your life you’ll get back.


8 Comments
Chris Buchanan
December 25, 2025 AT 10:36So let me get this straight - we’re telling older folks to spend $3K on a gadget that still can’t make sense of a restaurant conversation, but Medicare won’t cover it unless you’re on some fancy Advantage plan? Classic. I’ve seen my dad go through three pairs of hearing aids. The last one picked up his cat’s purr louder than my sister’s voice. At least the cat’s consistent.
And don’t get me started on the ‘OTC miracle’ hype. I bought a pair off Amazon for $400. They beeped when I sneezed. My dog started barking at them. I’m not saying they don’t help - I’m saying the system’s rigged to make you feel guilty for not buying your way back into the world.
Also, who designed these things? They look like tiny space radios that fell out of a 90s sci-fi movie. I’d rather just shout at my grandchildren until they learn sign language.
But hey - at least we’ve got apps that track how often I ‘engage socially.’ My hearing aid knows I haven’t talked to my wife in three days. Thanks, tech. Real helpful.
Wilton Holliday
December 26, 2025 AT 06:37Man, this post hit home. My mom went from ‘turning up the TV’ to ‘nodding through Thanksgiving dinner’ in like 18 months. We thought she was just being quiet - turns out she couldn’t hear half of what we were saying. We got her a Jabra Enhance last year. She cried the first time she heard her grandkid say ‘I love you’ without having to ask ‘what?’ five times.
She still hates the way they look - says they’re ‘like little ear bugs’ - but now she’s the one asking for the next family Zoom call. I swear, it’s like she got her social life back. The price was scary at first, but the 60-day trial made it feel safe. If you’re on the fence? Just try one. Even if you hate it, you’ll know for sure. And hey - your brain will thank you later. 💙
Raja P
December 27, 2025 AT 08:50Interesting read. In India, many elders just live with it - no testing, no devices. Some families think it’s ‘natural’ or even ‘spiritual’ - like God taking something away to teach patience. But I’ve seen how it isolates people. My uncle stopped going to temple because he couldn’t follow the chants. He started sitting alone, silent. No one realized how much he missed until he stopped laughing at jokes.
OTC aids are a game-changer here. Even the cheaper ones, if properly fitted, help more than nothing. The problem isn’t tech - it’s awareness. We need community health workers to talk about this like they do about diabetes. Not everyone can afford a $3K device, but $200? That’s doable.
Also - wind noise. Oh god, the wind noise. My aunt’s hearing aid sounds like she’s inside a tornado during monsoon season. Still better than silence, though.
Joseph Manuel
December 28, 2025 AT 14:30While the emotional appeal of this article is compelling, the data presented lacks sufficient contextualization. The 50% increased dementia risk statistic, for instance, is derived from observational studies that do not establish causation. Confounding variables - such as socioeconomic status, education level, and pre-existing cognitive decline - are not adequately controlled for in the cited literature.
Furthermore, the claim that hearing aids reduce dementia risk by 8–10% is extrapolated from a single longitudinal cohort study with a narrow demographic (primarily white, middle-class Americans). Generalizing this to a global population is methodologically unsound.
The assertion that OTC devices are ‘solid’ is equally misleading. Consumer Reports ratings are based on subjective user feedback, not clinical outcomes. The absence of professional fitting and real-time calibration renders many OTC models ineffective for sensorineural loss. This article reads less like a public health guide and more like a marketing brochure for hearing aid manufacturers.
Delilah Rose
December 30, 2025 AT 13:22Okay, so I’ve been thinking about this a lot since I read the article - not just because my dad has hearing loss, but because I’ve been noticing how quiet my own home has become. I mean, I’m 42, and I swear I’ve started asking people to repeat themselves too. Is it aging? Or is it just that we’ve all stopped listening? Like, really listening? We’re all so busy scrolling, talking over each other, trying to be heard - but no one’s actually hearing.
And then there’s the whole ‘hearing aids are expensive’ thing. I get it. But what if we treated hearing like vision? Like, if you need glasses, you get them. No one says, ‘Oh, you’re just getting old, squint harder.’ We don’t shame people for needing lenses. But hearing? We act like it’s a personal failure. Like if you just tried harder, you’d catch every word. But you can’t ‘try harder’ when your hair cells are gone. They’re not coming back.
And the fact that primary care docs don’t screen for it? That’s insane. We get yearly eye exams, dental cleanings, mammograms - but hearing? Nope. Not even a question. It’s like we’ve normalized silence as part of aging. But silence isn’t peaceful - it’s lonely. And loneliness kills faster than smoking. I’ve seen it. I’ve lived it. We need to stop treating hearing loss like a quiet problem. It’s loud. It’s screaming. And we’re not listening.
Also - I tried a hearing aid. For a week. It made everything too loud. Like, I could hear the fridge hum. I could hear my own breathing. I felt like I was trapped in a tin can. But after two weeks of adjustments? I heard my cat purr on the pillow next to me. And I cried. Not because it was perfect. But because I remembered what it felt like to be part of the world again.
So yeah. Get tested. Don’t wait. Even if you hate the device at first. Your brain will relearn. And so will your heart.
Aurora Daisy
January 1, 2026 AT 01:55Oh, so now we’re telling Americans they need to spend thousands on a gadget because they refuse to stop listening to their damn podcasts at 110 decibels since 2005? Classic. You let your ears rot from 15 years of noise pollution, then expect the government to fix it with a $3,000 earbud? Sorry, but I didn’t pay taxes so you could buy Bluetooth-enabled hearing aids to hear your TikTok notifications better.
And don’t get me started on the ‘OTC miracle’ nonsense. You think a $500 device from a website that doesn’t even have a physical address is going to fix what your own negligence destroyed? You didn’t protect your hearing, now you want a subsidy. Grow up.
Meanwhile, in the UK, we just say ‘speak up’ and move on. No apps. No trials. No corporate-sponsored ‘hearing loss is a public emergency’ campaigns. We just… live. And we’re still talking. Maybe you should too.
Also - dementia? Really? Next you’ll tell me that not wearing hearing aids causes global warming. Please.
Georgia Brach
January 1, 2026 AT 12:45The entire premise of this article is fundamentally flawed. The correlation between untreated hearing loss and dementia is misinterpreted as causation. Multiple meta-analyses, including those from the Journal of the American Medical Association, indicate that the association is likely mediated by social isolation and reduced cognitive stimulation - not auditory deprivation itself. To suggest that hearing aids reduce dementia risk by 8–10% is a gross oversimplification of complex neurodegenerative processes.
Furthermore, the promotion of OTC hearing aids is a regulatory failure disguised as consumer empowerment. These devices lack the calibration precision required for sensorineural hearing loss, which often requires individualized frequency response curves. The FDA’s 2022 decision was driven by lobbying, not evidence.
Additionally, the assertion that 85% of users report improved communication is based on self-reported surveys with no objective auditory testing. Placebo effect is significant in auditory perception. The entire narrative is a well-funded marketing campaign disguised as public health advocacy. Proceed with extreme skepticism.
Adarsh Dubey
January 1, 2026 AT 17:44I got my first hearing aid last year. Didn’t believe it would help. Turned out, I could hear my wife’s sighs again. Not the bad kind. The ‘I’m tired but still here’ kind. Small things matter.