GLP-1 Dose Titration Calculator
Calculate your personalized dose escalation timeline based on starting dose, target dose, and tolerance level. This tool helps visualize how slow dose adjustments can minimize side effects while reaching therapeutic goals.
The calculation is based on medical guidelines recommending 16-20 weeks for complete dose escalation. Results are for informational purposes only.
| Week | Dose (mg) | Side Effect Risk |
|---|
When you hear about GLP-1 drugs, you might think of weight loss headlines or celebrity endorsements. But behind the buzz are real medicines with complex safety profiles - and the next generation is changing everything. These aren’t just improved versions of older drugs. They’re multi-targeted, longer-lasting, and more potent. And with that power comes new questions: How safe are they really? What side effects should you watch for? And why do some people stop taking them before they even feel the benefits?
What Makes a GLP-1 Agent ‘Next-Generation’?
First-generation GLP-1 receptor agonists like liraglutide and semaglutide work by mimicking a natural hormone that tells your body to release insulin, slow digestion, and feel full. They helped millions lose weight and control blood sugar. But they had limits - daily or weekly injections, moderate weight loss (around 10-15%), and stubborn side effects like nausea.
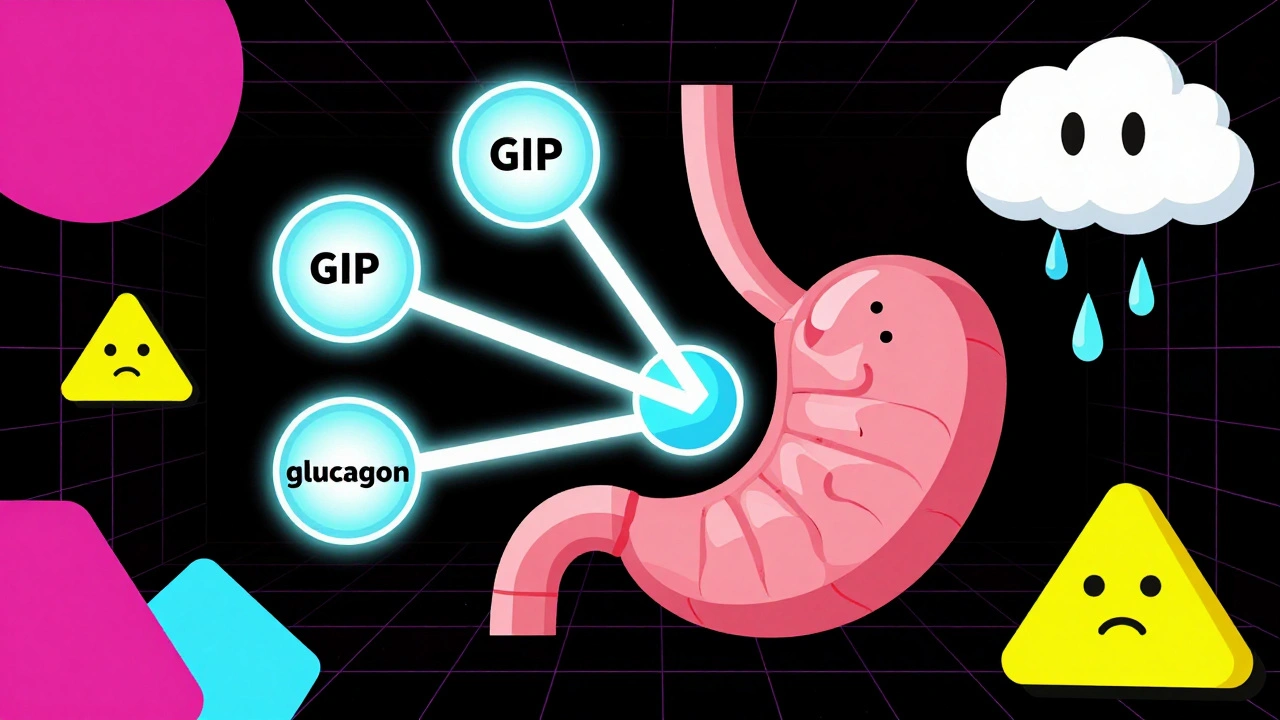
Next-generation agents go further. They don’t just activate one receptor. They hit two or even three at once. Retatrutide, from Eli Lilly, is a triple agonist: it targets GLP-1, GIP, and glucagon receptors. In Phase II trials, people lost up to 24.2% of their body weight after 48 weeks. That’s not a small change - it’s life-altering. Orforglipron, an oral pill, isn’t injected at all. In trials, it led to 15-20% weight loss, with waistlines shrinking by nearly 10 cm. VK2735, another dual agonist, hit nearly 15% weight loss in just 13 weeks.
These aren’t just stronger versions. They’re smarter. By activating multiple pathways, they may improve fat burning, energy use, and appetite control more effectively. But that also means the body reacts differently - and sometimes more intensely.
The Most Common Side Effects: It’s Still the Gut
Despite all the innovation, the biggest problem hasn’t gone away. Nausea, vomiting, diarrhea, and constipation are still the most common side effects. In fact, according to the 2025 American Diabetes Association Standards of Care, 30-50% of patients on any GLP-1 therapy report gastrointestinal issues. Even with dual and triple agonists like retatrutide and VK2735, these side effects haven’t improved much. A 2025 study in PubMed found that adding more receptors didn’t reduce stomach problems - it just added more weight loss.
Here’s what most people experience:
- Nausea: Affects 20-35% of users, especially when starting or increasing the dose.
- Vomiting: Seen in 5-15%, more common at higher doses.
- Diarrhea and constipation: Each affects 10-20% of patients, often alternating.
Most of these symptoms fade after 4-8 weeks. But about 5-10% of people stop treatment because the side effects are too uncomfortable. That’s why dose titration matters. Doctors now recommend slowly increasing the dose over 16-20 weeks. Rushing it doesn’t make results come faster - it just makes nausea worse.
What You Don’t Hear About: Muscle, Bone, and Long-Term Risks
Weight loss sounds great - until you lose muscle instead of fat. That’s a real concern with rapid, large-scale weight loss. Dr. Daniel J. Drucker, a leading researcher at the University of Toronto, warns that next-generation agents causing over 20% weight loss could impact muscle mass and bone density. We don’t have five-year data yet. But early signs show that without careful nutrition and resistance training, people may lose lean tissue - not just fat.
Pancreatitis remains a theoretical risk. The American Gastroenterological Association still recommends monitoring for abdominal pain, especially in those with a history of pancreas issues. While no clear link has been proven in trials, the concern hasn’t been ruled out.
And then there’s the long game. What happens after 5 or 10 years of using these drugs? Will the body adapt? Will nutrient absorption change? Will bone density drop? Dr. Elena Grunvald, lead author of the AGA guidelines, says we simply don’t know yet. Clinical trials last 1-2 years. Real-world use lasts decades. That gap is growing.

Oral GLP-1s: A Game-Changer - But Not Without Risks
Orforglipron is the first oral GLP-1 agonist to show serious results. No needles. No injections. Just a pill. That’s huge for people who hate needles or struggle with adherence. In trials, it lowered systolic blood pressure by 4.2 mm Hg and diastolic by 1 mm Hg - a bonus for heart health.
But the side effect profile? It’s almost identical to injectables. Nausea, bloating, and changes in bowel habits are still common. And because it’s absorbed through the gut, there’s a chance for drug interactions or absorption issues in people with gut conditions like Crohn’s or celiac disease. More research is needed on how it behaves in real-world populations - especially older adults or those with liver or kidney issues.
The Hidden Danger: Compounded GLP-1 Products
There’s a dark side to this revolution. Online pharmacies and compounding clinics are selling non-FDA-approved versions of semaglutide and tirzepatide. These aren’t regulated. They’re not tested. And they’re dangerous.
The University of Illinois at Chicago’s Digital Pharmacy issued a warning in August 2025: compounded GLP-1 products have caused serious adverse events - including hospitalizations - due to inconsistent dosing and impurities. One patient reported severe vomiting and dizziness after taking a compounded version that turned out to be 30% stronger than labeled. Another developed an allergic reaction to a filler not found in FDA-approved versions.
Doctors are now trained to ask: “Are you using a pharmacy that follows USP <795> standards?” If the answer is no, they’re advised to stop the medication immediately. The FDA has issued multiple alerts since 2024. These aren’t “cheaper alternatives.” They’re risky bets.
Who Should Be Cautious?
Not everyone is a good candidate. People with:
- A personal or family history of medullary thyroid cancer or MEN2 syndrome
- Severe gastrointestinal disorders like gastroparesis
- History of pancreatitis
- Significant kidney or liver impairment
- Those planning pregnancy or breastfeeding
should talk to their doctor before starting. Even if they’re healthy, rapid weight loss can unmask hidden conditions - like gallstones, which are more common after losing more than 10% of body weight quickly.
What’s Coming Next?
Retatrutide’s Phase III trials wrap up in late 2025 or early 2026. Results will include detailed safety data on muscle mass, bone density, and cardiovascular outcomes. VK2735’s Phase III trials are moving faster than expected. Merck’s danuglipron is also in late-stage testing.
Researchers are now looking beyond weight loss. GLP-1 agents are being tested for fatty liver disease, Parkinson’s, Alzheimer’s, and even heart failure. Each new use brings new safety questions. Will these drugs affect brain function in older adults? Could they interact with antidepressants? What happens if someone stops after five years?
One thing is clear: the future of GLP-1 therapy isn’t just about losing weight. It’s about losing weight safely, sustainably, and without unintended harm.
What Should You Do?
If you’re considering a next-generation GLP-1 agent:
- Only use FDA-approved versions - avoid compounded products at all costs.
- Ask your doctor about dose titration. Don’t rush to the highest dose.
- Track your symptoms. Keep a journal of nausea, bowel changes, energy levels.
- Get baseline blood tests for liver, kidney, and vitamin levels before starting.
- Work with a dietitian. Protein intake and resistance training are critical to protect muscle.
- Ask about long-term monitoring. This isn’t a short-term fix.
These drugs are powerful. But they’re not magic. They work best when paired with lifestyle changes - not instead of them.

13 Comments
Taya Rtichsheva
December 9, 2025 AT 13:08so like... glp-1s are just fancy diet pills now huh? 🤡
Lola Bchoudi
December 10, 2025 AT 20:53The multi-receptor agonism in next-gen agents like retatrutide represents a paradigm shift in metabolic pharmacology-simultaneous GLP-1/GIP/glucagon co-activation enhances satiety signaling, hepatic gluconeogenesis suppression, and lipolysis induction beyond monoreceptor targeting. However, the GABAergic and vagal afferent cross-talk may exacerbate nausea via central and enteric nervous system overstimulation, which explains why GI adverse events persist despite improved efficacy.
Andrea Petrov
December 12, 2025 AT 07:45You know... I’ve been reading about how Big Pharma is quietly pushing these drugs to replace actual nutrition science. They don’t want you to eat real food-they want you dependent on a $1000/month injection. And the FDA? Totally asleep at the wheel. Compounded versions are the only way to get real dosing-why else would they ban them? Something’s fishy.
Suzanne Johnston
December 13, 2025 AT 18:15There’s an existential layer here that’s rarely acknowledged: if we’re optimizing the body for weight loss through pharmacological coercion, what does that say about our relationship with selfhood? Are we becoming machines to be tuned, or are we still human beings with needs beyond metabolic metrics? The science is brilliant-but the cultural surrender to pharmaceutical solutions feels like a quiet tragedy.
Christian Landry
December 14, 2025 AT 13:04i tried orforglipron for 3 wks and yeah the nausea was wild at first but after 2 weeks it got way better. still lost 8 lbs and my jeans fit lol 🤘
Graham Abbas
December 14, 2025 AT 14:19I remember when we used to lose weight by walking and eating less. Now we need triple-receptor agonists and a PhD in pharmacology just to take a pill. This isn’t progress. This is surrender. And yet... I still want one. 😭
Haley P Law
December 15, 2025 AT 16:10I lost 20 lbs in 12 weeks on retatrutide and I’m basically a new person. My anxiety dropped. My skin cleared. My husband said I looked ‘like I had a glow-up from a rom-com’. I’m not sorry. 🌟
Andrea DeWinter
December 17, 2025 AT 06:23if you start these make sure you get your vit d b12 and magnesium checked before and after. muscle cramps hit hard if you dont and people dont talk about it enough
George Taylor
December 17, 2025 AT 23:25Let’s be honest: 50% of users have GI side effects? That’s not ‘common’-that’s a dealbreaker. And yet, everyone’s acting like this is a miracle cure. Who’s funding these trials? Who’s getting rich? And why are we ignoring the fact that this isn’t medicine-it’s a lifestyle brand with a prescription pad?
Nikhil Pattni
December 18, 2025 AT 11:38Actually, I think people are missing the point. In India, we’ve been using traditional herbs like fenugreek and berberine for centuries to modulate GLP-1 pathways naturally. These synthetic drugs are just Western rebranding of ancient physiology. Plus, the long-term gut microbiome disruption is going to be catastrophic-especially with oral formulations bypassing normal bile acid cycling. I’ve seen 3 patients with post-GLP-1 SIBO. No one’s studying this.
Arun Kumar Raut
December 20, 2025 AT 05:40just take it slow. start low. eat protein. move your body. drink water. youll be fine. no need to overthink it
Darcie Streeter-Oxland
December 21, 2025 AT 03:03The pharmacoeconomic implications of widespread adoption of next-generation GLP-1 agonists are profoundly concerning. The marginal utility of an additional 5% weight loss must be weighed against the exorbitant cost of treatment, the strain on healthcare infrastructure, and the potential for iatrogenic muscle atrophy. A cost-benefit analysis, conducted with appropriate methodological rigour, has yet to be published in a peer-reviewed journal of repute.
Steve Sullivan
December 22, 2025 AT 14:37i get why people hate the nausea but honestly? it’s the price of admission. i went from 280 to 190. my knees don’t hurt anymore. my sleep’s better. yeah i puked a few times. worth it. 🙌