When you’re overweight or obese, your body doesn’t just carry extra weight-it changes how medicines work. A standard dose that works perfectly for someone with a normal weight might be too low, too high, or just plain ineffective in someone with obesity. This isn’t about being ‘big’ or ‘small.’ It’s about biology. Fat changes how drugs move through your body, where they go, how long they last, and how strongly they act. And if doctors don’t adjust for that, patients are at risk of treatment failure, side effects, or even life-threatening complications.
Why Standard Dosing Fails in Obesity
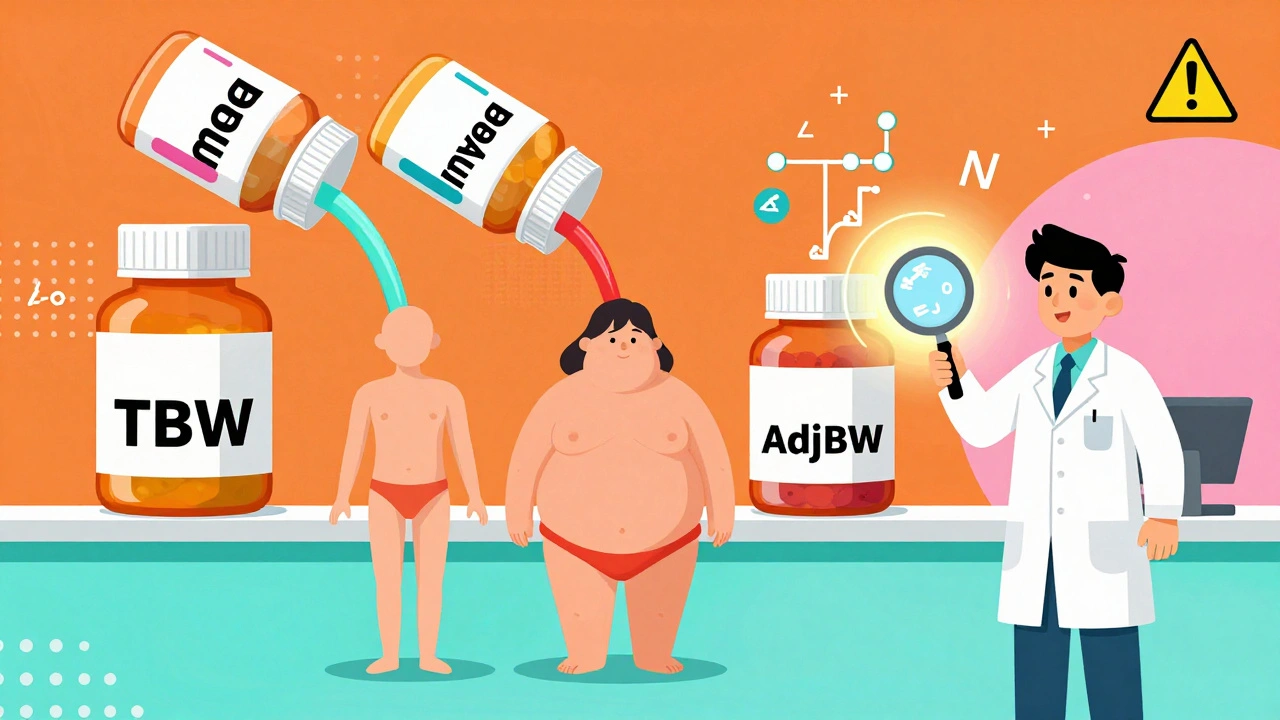
Most drug labels still list dosing based on total body weight (TBW)-the number you see on the scale. But in obesity, that number doesn’t tell the full story. About 39.8% of U.S. adults have obesity, according to CDC data from 2016, and that number has only grown since. Yet most medications were tested in people with average body weight. The result? A mismatch. Obesity increases fat tissue, which can be up to 50% of total body mass in Class III obesity (BMI ≥40). That fat isn’t just padding-it’s an active tissue that absorbs certain drugs. Lipophilic drugs like diazepam or clindamycin dissolve easily in fat. In someone with obesity, these drugs spread out more, lowering their concentration in the blood. If you give the same dose as a normal-weight person, the drug might never reach the level needed to work. On the flip side, hydrophilic drugs-like many antibiotics-don’t mix well with fat. They stay mostly in blood and fluid. But obesity also increases blood volume and kidney function. That means these drugs get cleared faster. A 1g dose of cephazolin, standard for surgical prophylaxis, often falls below therapeutic levels in obese patients. Studies show up to 42% higher clearance. That’s why many hospitals now give 2g instead.Lean Body Weight vs. Total Body Weight: What’s the Difference?
The key to better dosing is using the right weight metric. Here’s what matters:- Total Body Weight (TBW): What the scale says. Often too high for hydrophilic drugs, too low for lipophilic ones.
- Ideal Body Weight (IBW): A calculated estimate of what weight you should be based on height and sex. Used for drugs that don’t go into fat.
- Lean Body Weight (LBW): The weight of your muscles, organs, and bones-everything except fat. Best for lipophilic drugs.
- Adjusted Body Weight (AdjBW): A hybrid formula that blends TBW and IBW. Used widely for antibiotics.
The most common formula for AdjBW is: AdjBW = IBW + 0.4 × (TBW - IBW)
For example, a man who is 5’10” and weighs 130kg has an IBW of about 75kg. His AdjBW would be 75 + 0.4 × (130 - 75) = 97kg. That’s the weight you’d use to calculate his antibiotic dose-not his full 130kg.
Using TBW for drugs like vancomycin or aminoglycosides leads to dangerously high levels. Using IBW alone for drugs like enoxaparin leaves patients unprotected. The right tool depends on the drug-and the patient.
Antibiotics: Where the Rules Are Clearest
Antibiotics are where obesity dosing is most studied-and where mistakes are most dangerous. A subtherapeutic level doesn’t just mean a slow recovery. It can lead to resistant infections, longer hospital stays, or death.- Ceftriaxone: Standard dose is 1g daily. In obese patients (BMI >30), that dose results in subtherapeutic troughs in 63% of cases. The fix? Minimum 2g daily. UCSF’s protocol reduced surgical infections from 14.2% to 8.7% after making this change.
- Vancomycin: Dosing by TBW leads to supratherapeutic levels in 39% of obese patients. Therapeutic drug monitoring (TDM) is now recommended by IDSA. Target trough: 15-20 mg/L.
- Colistin: Toxic to kidneys. Maximum daily dose capped at 360mg colistin base activity (CBA) or 12 million units (MU) of colistimethate sodium-based on IBW, not TBW. Nephrotoxicity hits 44% in obese patients if dosed wrong.
- Tigecycline: Standard loading dose is 100mg, then 50mg every 12 hours. But for resistant Gram-negative infections, newer data supports 200mg loading, then 100mg every 12 hours-regardless of weight.
These aren’t guesses. They’re backed by TDM studies, clinical trials, and hospital outcomes. Stanford Health Care cut supratherapeutic vancomycin levels from 39% to 12% after switching to AdjBW dosing. That’s not a small win-it’s a lifesaver.
Anticoagulants: The High-Stakes Game of Dosing
Enoxaparin (Lovenox) is one of the most misunderstood drugs in obesity. It’s used to prevent blood clots after surgery or during hospital stays. But here’s the catch: fixed doses don’t work.- BMI 40-49.9: 40mg twice daily
- BMI ≥50: 60mg twice daily
Why? A 2018 JAMA Surgery trial showed 40mg twice daily reduced blood clots by 37% in obese patients. But if you give 20mg (the standard dose), it only drops clots by 20%. That’s a 17% gap in protection. And if you give 40mg to someone with BMI 52? You’re still underdosing. Studies show 21% of these patients have subtherapeutic anti-Xa levels.
And then there’s apixaban (Eliquis). This one’s worse. It uses a rigid 85kg cutoff: 5mg twice daily if under 85kg, 10mg if over. But this creates a brutal discontinuity. Patients just above 85kg get a 100% dose jump. Medicare data shows those patients have a 47% higher bleeding risk than those just below the line. It’s not science-it’s a cliff edge.
Metoprolol, by contrast, uses continuous weight-based dosing (5mg per kg up to 200kg). No jumps. No cliffs. Just smooth, predictable levels. Why don’t more drugs follow that model?
Therapeutic Drug Monitoring: The Missing Link
You can’t guess your way to the right dose in obesity. You need data. Therapeutic Drug Monitoring (TDM) measures actual drug levels in the blood. It’s not optional anymore for drugs like vancomycin, voriconazole, aminoglycosides, and some antifungals in obese patients. Stanford’s 2022 TDM study found that dosing voriconazole by TBW led to supratherapeutic levels in 39% of obese patients. Switching to AdjBW cut that to 12%. That’s a 70% drop in toxicity risk. Yet only 37% of U.S. hospitals have formal obesity dosing protocols. And only 63% of pharmacists say their institutions support TDM programs. That’s a gap between evidence and practice. TDM isn’t just for ICU patients. It’s for anyone with BMI >30 on critical drugs. It’s fast. It’s accurate. And it’s cheaper than treating a failed infection or a kidney injury from overdose.What’s Holding Back Better Dosing?
The science is clear. The guidelines exist. So why do so many patients still get the wrong dose?- Outdated labels: Only 18% of FDA-approved drug labels include obesity-specific dosing advice.
- Training gaps: A 2021 University of Michigan study found 43% of internal medicine residents didn’t know when to use IBW vs. TBW. That led to 28% dosing errors.
- System barriers: Electronic health records often don’t auto-calculate AdjBW. Pharmacists have to do it manually-time-consuming, error-prone.
- Cost and access: TDM isn’t available everywhere. Community pharmacies rarely offer it. Academic centers do. That creates a two-tier system.
At Mayo Clinic, they fixed this by building an EHR alert system. When a doctor orders vancomycin for a patient with BMI >30, the system flags it and suggests a weight-based calculation. Result? Subtherapeutic levels dropped from 31% to 9%. Length of stay fell by 2.3 days. That’s not just better care-it’s better economics.
What You Can Do Right Now
If you’re a patient with obesity:- Ask: “Is my dose based on my actual weight or my ideal weight?”
- Ask: “Has my drug level been checked?”
- Ask: “Is there a better way to dose this for someone with my body type?”
If you’re a clinician:
- Use AdjBW for antibiotics. Use LBW for lipophilic drugs. Use IBW for hydrophilic drugs.
- Don’t rely on total body weight unless the drug is proven safe that way.
- Push for TDM access in your hospital. Start with vancomycin or voriconazole.
- Use the Clincalc.com Obesity Dosing Reference-it’s updated weekly and covers 147 drugs.
There’s no one-size-fits-all. But there is a better way. It’s not about guessing. It’s about measuring. It’s not about tradition. It’s about science.
What’s Next for Obesity Dosing?
The future is personal. The NIH just funded a $4.7 million study tracking 500 obese patients over five years to map how drugs behave across different body compositions. The FDA now requires obesity subgroups in new drug trials. And companies like DoseMe in Australia are using AI and Bayesian modeling to predict exact doses based on weight, kidney function, and genetics. Soon, dosing won’t just be based on BMI. It’ll be based on muscle mass, fat distribution, liver function, and even your genes. Imagine a scan that shows your body’s drug storage zones-and a program that tells your doctor the exact dose to give. That’s not sci-fi. It’s coming.For now, we have what we need: formulas, data, and guidelines. What’s missing is consistent use. Every patient with obesity deserves a dose that fits-not one that’s just convenient.

12 Comments
nikki yamashita
December 13, 2025 AT 08:46This is such a needed conversation. I had a friend who got sepsis after surgery because they gave her the standard antibiotic dose-she had BMI 45 and it was completely ineffective. No one even thought to adjust it. 😔
Robert Webb
December 15, 2025 AT 07:41It’s wild how medicine still operates like it’s 1995. We’ve got body composition scans, AI-driven pharmacokinetic models, and real-time TDM-but most hospitals still just eyeball dosing based on a number on a scale. The disconnect between what we know and what we do isn’t just lazy-it’s lethal. We’re not treating patients; we’re treating BMI brackets. And that’s not science. That’s guesswork with a white coat.
Look at vancomycin. The data’s been clear for over a decade. Adjusted body weight reduces toxicity and improves outcomes. Yet pharmacists are still manually calculating doses in Excel sheets because the EHR won’t auto-populate it. This isn’t a knowledge gap. It’s a systems failure. And until we fix the infrastructure, we’re just rearranging deck chairs on the Titanic.
Also, the apixaban 85kg cliff? That’s not dosing. That’s a glitch in the matrix. Someone at Pfizer thought, ‘Let’s make a hard cutoff because it’s easy to code.’ Not because it’s safe. Not because it’s smart. Just because it’s convenient. And now patients are bleeding out because of a programming decision. That’s not malpractice. That’s negligence dressed in algorithm.
We need mandatory obesity pharmacology modules in med school. We need EHR alerts that scream when you try to order 40mg of enoxaparin for someone with BMI 52. We need TDM to be as routine as checking blood pressure. And we need the FDA to stop approving drugs without obesity subgroups. This isn’t niche. It’s 40% of the population. If we can’t dose them right, we shouldn’t be prescribing at all.
Laura Weemering
December 17, 2025 AT 00:52So… let me get this straight. We’ve got decades of peer-reviewed studies showing that fat tissue alters drug distribution, and yet we’re still giving people the same dose as a 150lb person? And you’re telling me the FDA hasn’t updated 82% of labels? That’s not negligence-it’s institutional cruelty. Who’s getting rich off this? Pharma? Hospitals? The billing departments that don’t want to code for TDM? Someone’s making money off this ignorance, and it’s not the patients.
And don’t even get me started on ‘ideal body weight.’ Who decided that? Some 1950s doctor with a slide rule and a moral panic about ‘obesity’? IBW is a fantasy. It’s not a biological truth. It’s a cultural judgment wrapped in math. And now we’re killing people with it.
I’m not even mad. I’m just… exhausted.
Audrey Crothers
December 18, 2025 AT 19:54OMG YES. I’m a nurse and this is EVERY DAY. I had to argue with a resident last week because he ordered 40mg Lovenox for a patient with BMI 54. I pulled up the JAMA study and he still said ‘but the chart says 40.’ I had to call the pharmacy director. 😤 We need a crash course for every doc. Like, a 10-minute video they HAVE to watch before prescribing. PLEASE.
Also-Clincalc.com is a GODSEND. Bookmark it. Now.
Nathan Fatal
December 19, 2025 AT 22:52There’s a reason why ICU mortality is higher in obese patients on antibiotics-it’s not the obesity. It’s the dosing. We’re not treating the disease. We’re treating the scale. And that’s why sepsis survival rates are worse for this group. The data doesn’t lie. The system does.
AdjBW isn’t a suggestion. It’s standard of care. If your hospital doesn’t use it for vancomycin, aminoglycosides, or ceftriaxone in BMI >30, they’re practicing below the standard. That’s not opinion. That’s legal risk.
And yes, TDM should be routine. Not ‘if you can get it.’ Routine. Like glucose checks. Like EKGs. It’s not expensive. It’s life-saving. Stop treating it like a luxury.
Also, the apixaban cliff? That’s a design flaw. Not a medical one. Someone at Bristol Myers Squibb wrote a hard-coded if-statement and didn’t think it through. That’s not science. That’s software engineering with zero clinical input. And now people are dying because of a bug.
sandeep sanigarapu
December 20, 2025 AT 03:12Excellent summary. In India, this issue is even more acute. Many patients are undernourished but also have visceral obesity. Standard dosing fails both groups. We need localized guidelines. Not just Western formulas. Weight alone is not enough. Muscle mass matters. Liver function matters. We must move beyond BMI.
Thank you for highlighting TDM. It is not a luxury. It is essential.
Ashley Skipp
December 20, 2025 AT 13:16Ugh. Another ‘obesity is a disease’ article. You know what causes bad dosing? Bad doctors. Not fat people. Stop making excuses for incompetence. Just teach them to use the damn formulas. And stop pretending this is some revolutionary insight. It’s not. It’s basic pharmacology.
Also, why is everyone acting like this is new? We’ve known this since the 80s. Grow up.
wendy b
December 22, 2025 AT 04:07Okay but… what if this is all just a ploy to sell more TDM kits and AI dosing software? Pharma’s been pushing ‘personalized medicine’ for 20 years. Meanwhile, insulin prices tripled. Who’s really benefiting? Not me. Not my cousin who got kidney failure from vancomycin. Not the guy who got a clot because they gave him 20mg Lovenox. It’s the tech companies. The labs. The consultants. This isn’t science. It’s a profit pipeline wrapped in jargon.
And don’t get me started on ‘AdjBW.’ That’s just a fancy way of saying ‘we don’t know what to do so let’s make up a number.’
Why not just test everyone’s drug levels before giving a dose? Oh right. Because it’s expensive. And they’d rather you die quietly than pay for a blood test.
Wake up. This isn’t about medicine. It’s about money.
Lawrence Armstrong
December 23, 2025 AT 03:37Just had a patient today with BMI 48. Ordered vancomycin. Used AdjBW. Got a TDM result back-perfect trough. She’s walking out tomorrow. No kidney damage. No infection. Just science working.
It’s not magic. It’s math. And it works. 🤝
Donna Anderson
December 24, 2025 AT 17:25i just learned about adjbw yesterday and now i’m mad at every doctor i’ve ever had 😭 why didn’t anyone tell me this? my cousin died from a clotted lung and they gave her the regular dose… i think it was because she was ‘big’ and they didn’t wanna ‘overdose’ her… but it was the opposite.
pls share this. everyone needs to know.
Nathan Fatal
December 25, 2025 AT 21:33That’s exactly why we need mandatory EHR alerts. Not just for vancomycin. For everything. Enoxaparin. Ceftriaxone. Tigecycline. If the system doesn’t flag it, doctors won’t think about it. And if they don’t think about it, patients die. We’re not talking fringe cases. We’re talking 1 in 2.5 hospital admissions. That’s not rare. That’s epidemic. And the fix? It’s already built. It’s just not turned on.
Stop blaming doctors. Fix the system.
Robert Webb
December 27, 2025 AT 03:59And if you’re a patient reading this? Don’t wait for your doctor to know this. Ask. Specifically. ‘Is my dose calculated using adjusted body weight?’ If they look confused? That’s your sign. Walk out. Get a second opinion. Your life isn’t a guess. It’s a calculation. And you deserve the right numbers.
Also, if you’re a student, learn this now. Don’t wait until you’re prescribing. This is the difference between being a technician and being a healer.