When you’re living with rheumatoid arthritis, psoriatic arthritis, or Crohn’s disease, the pain and fatigue can feel endless. Then comes a TNF inhibitor-like Humira, Enbrel, or Remicade-and suddenly, you can get out of bed, play with your kids, or walk to the store without collapsing. But then you hear it: "TNF inhibitors might increase your cancer risk." That one sentence can turn relief into fear. So, what’s real? What’s hype? And what should you actually do?
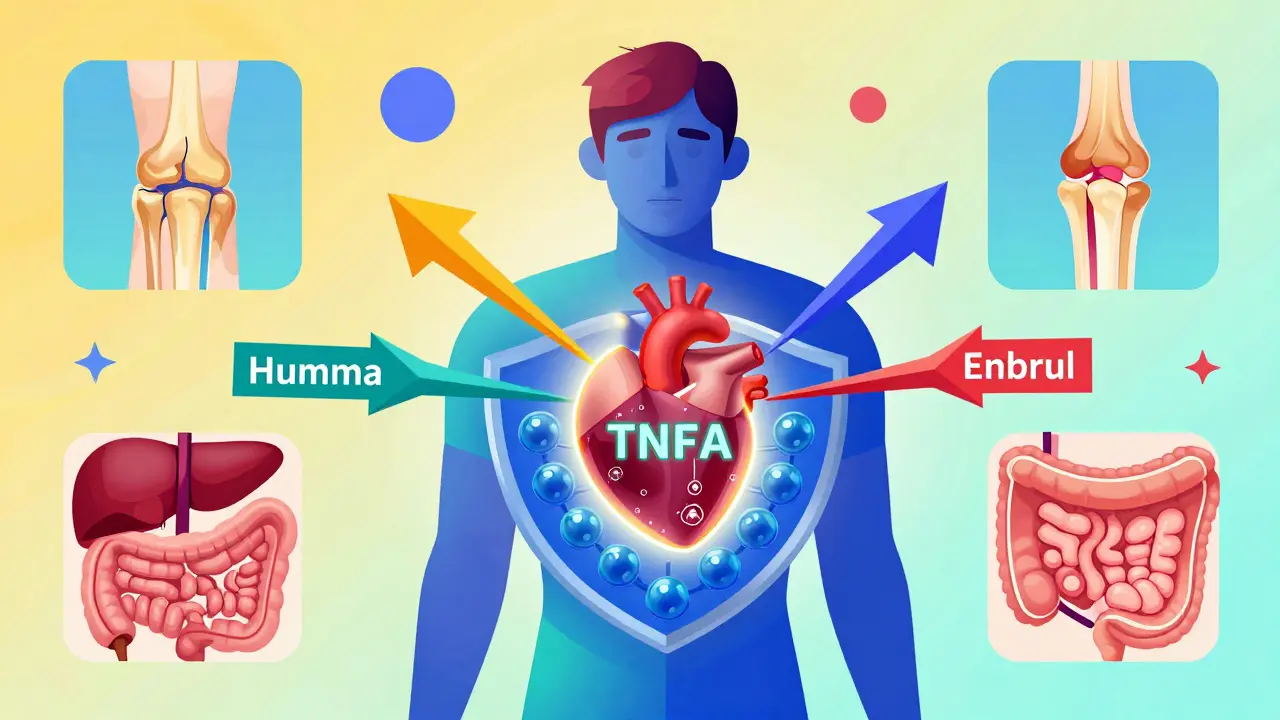
What Are TNF Inhibitors, Really?
TNF inhibitors are a type of biologic drug designed to block tumor necrosis factor-alpha (TNF-α), a protein that drives inflammation in autoimmune diseases. Think of TNF-α like a fire alarm that’s stuck on-your immune system is attacking your own joints, skin, or gut, and this protein is the alarm bell ringing nonstop. TNF inhibitors quiet that alarm.
Five are approved in the U.S.: infliximab, etanercept, adalimumab, certolizumab, and golimumab. They’re not pills. You inject them under your skin or get them through an IV. Some you take weekly, others every few weeks. They cost between $4,500 and $6,500 a month. That’s not cheap. But for many, it’s life-changing. Around 1.5 million Americans use them. And they work-50 to 70% of patients see major improvement in symptoms within six months.
But here’s the catch: by turning down inflammation, you’re also turning down part of your immune system’s ability to spot and kill abnormal cells. That’s immunosuppression. And that’s where the cancer question starts.
The Cancer Risk: What the Data Actually Shows
The fear of cancer from TNF inhibitors isn’t made up. Back in 2012, a big study in JAMA found that monoclonal antibody TNF inhibitors-like adalimumab and infliximab-were linked to a nearly threefold higher risk of cancer compared to placebo. That sent shockwaves through the medical world.
But that study looked at short-term trials. Real life is longer. And real-world data tells a different story.
A 2022 Swedish study tracking over 15,700 rheumatoid arthritis patients for up to 12 years found no overall increase in cancer risk with TNF inhibitors compared to older, non-biologic drugs. In fact, etanercept showed a slightly lower risk. Adalimumab? It had a small spike in the first year-but experts now think that’s not because it causes cancer. It’s because people with undiagnosed cancer were more likely to start it. Their symptoms (fatigue, weight loss) looked like worsening arthritis. That’s called protopathic bias.
For skin cancer, the picture is clearer. Multiple studies show a 30% higher risk of non-melanoma skin cancer (basal cell and squamous cell carcinomas) in patients using TNF inhibitors, especially adalimumab. One 2021 meta-analysis found adalimumab users had 1.3 times the risk of skin cancer compared to etanercept users. That’s not huge-but it’s real.
And here’s something surprising: a 2023 study of 1,872 cancer patients with rheumatoid arthritis found those on TNF inhibitors had better survival rates after lung cancer diagnosis than those on older drugs. Their 3-year survival was 42% higher. Why? Maybe because TNF inhibitors helped control inflammation that was helping the cancer grow. Or maybe because they were healthier overall. We don’t know yet.
What About Lymphoma?
Lymphoma is the big scary word. The FDA added a black box warning for lymphoma in 2008. And yes, there’s a small increase in risk-especially in young people with very active disease, or those on high-dose steroids. But here’s the key: the absolute risk is still very low. For every 10,000 patients on TNF inhibitors, about 1 to 2 extra cases of lymphoma occur per year. Compare that to the general population: about 0.5 cases per 10,000. So, yes, it’s higher. But it’s still rare.
And here’s the twist: patients with severe, untreated rheumatoid arthritis have a higher baseline risk of lymphoma than those on TNF inhibitors. Controlling the disease might be the best way to lower your cancer risk long-term.
Who Should Be Worried?
Not everyone. The biggest red flags are:
- History of melanoma or other skin cancers
- Previous lymphoma or blood cancer
- Current smoking
- High-dose steroids (over 7.5 mg of prednisone daily)
- Age over 65
If you’ve had a low-risk cancer-like early-stage breast, prostate, or colon cancer-most rheumatologists will restart a TNF inhibitor after you’ve been cancer-free for 2 to 5 years, depending on the cancer type. A 2023 registry study found 87% of doctors continued TNF inhibitors in these patients with no new cancer events.
But if you’ve had melanoma or lymphoma? That’s trickier. Many doctors avoid TNF inhibitors entirely. The risk isn’t zero. And we don’t have enough long-term data to say it’s safe.
What Should You Do Before Starting?
Before you get your first shot, your rheumatologist should:
- Check your skin thoroughly for suspicious moles or lesions
- Order age-appropriate cancer screenings (mammogram, colonoscopy, etc.)
- Ask about your personal and family cancer history
- Discuss your smoking status and whether you’re ready to quit
- Review your steroid use-if you’re on more than 7.5 mg of prednisone daily, they should be trying to taper you off
And here’s the one thing most patients forget: your dermatologist should be part of the team. If you’re on a TNF inhibitor, get a full-body skin check every 6 to 12 months. That’s not optional. It’s part of your treatment plan.
What About the Future?
Things are changing fast. By 2027, doctors may use genetic tests to predict who’s at higher risk for lymphoma while on TNF inhibitors. A 2023 study in Nature Genetics found certain gene patterns could identify patients with 3.2 times higher risk. That means we might soon be able to say: “You’re low risk-go ahead.” Or: “You’re high risk-let’s try something else.”
And the drugs themselves are evolving. Newer biologics-like JAK inhibitors and IL-17 blockers-are gaining ground. But they’re not better when it comes to cancer risk. Some may be worse. TNF inhibitors still have the longest safety track record-20 years of data showing no cumulative increase in cancer risk over time.
Real Stories, Real Choices
One patient from the Rheumatology subreddit wrote: “I got diagnosed with basal cell carcinoma on my nose after 18 months on Humira. I had it removed. My rheumatologist said I could restart it. I did. I’ve been cancer-free for 2 years. I’d do it again.”
Another said: “I had lymphoma at 32. I’m in remission. My doctor won’t let me go back on Enbrel. I miss the life I had before. I feel like I’m punished for being sick.”
There’s no one-size-fits-all answer. But here’s what the data says: for most people, the benefits of TNF inhibitors outweigh the risks. The risk of uncontrolled inflammation-joint destruction, heart disease, lung damage-is far greater than the small, manageable risk of cancer.
And if you’re scared? Talk to your rheumatologist. Ask for the data. Ask about your skin checks. Ask if you can switch to etanercept if you’re on adalimumab and worried about skin cancer. Ask if your steroid dose can be lowered.
You don’t have to choose between pain and cancer. You can have both controlled-if you’re informed, monitored, and partnered with your care team.

What If You’ve Already Started?
Don’t panic. Don’t stop. But do this:
- Check your skin every month. Use a mirror. Look for new moles, sores that don’t heal, or patches that are red, scaly, or growing.
- See your dermatologist every 6 months. Even if you feel fine.
- Report any unexplained weight loss, night sweats, or swollen lymph nodes right away.
- Keep your cancer screenings up to date.
- Don’t smoke. Ever.
- Ask your doctor if you can switch to etanercept if you’re on adalimumab and have a history of skin cancer.
Most people on TNF inhibitors never get cancer because of them. But those who do? Often, it’s caught early-because they were watching.
Bottom Line
TNF inhibitors don’t cause cancer in the way people fear. They don’t turn your body into a cancer factory. But they do slightly increase your risk of certain cancers-mainly skin cancer and, rarely, lymphoma. That risk is small. It’s manageable. And it’s far lower than the risk of letting your autoimmune disease run wild.
The real danger isn’t the drug. It’s silence. It’s skipping skin checks. It’s ignoring symptoms. It’s assuming the worst without checking the facts.
If you’re on a TNF inhibitor, you’re not taking a gamble. You’re managing a known, monitored risk. And for millions, it’s the difference between living and surviving.
Do TNF inhibitors cause cancer?
TNF inhibitors do not directly cause cancer. However, they slightly increase the risk of certain cancers-especially non-melanoma skin cancer and, rarely, lymphoma. This is because they suppress part of the immune system that normally detects and destroys abnormal cells. The absolute risk remains low, and long-term studies show no overall increase in cancer deaths among users.
Is adalimumab riskier than etanercept for cancer?
Yes, for skin cancer. Multiple studies show adalimumab carries about a 30% higher risk of non-melanoma skin cancer compared to etanercept. This is likely due to differences in how the drugs bind to TNF-alpha. Etanercept has shown either no increased risk or even a slightly lower risk than not using biologics at all. If you’re concerned about skin cancer, switching to etanercept may be a safer option.
Can I take TNF inhibitors if I’ve had cancer before?
It depends on the type and stage of cancer. For low-risk cancers like early-stage breast or prostate cancer, most rheumatologists will restart TNF inhibitors after 2 to 5 years of being cancer-free. For melanoma or lymphoma, most avoid them entirely due to insufficient safety data. Always consult your oncologist and rheumatologist together before restarting.
How often should I get skin checks?
If you’re on a TNF inhibitor, get a full-body skin exam by a dermatologist every 6 to 12 months. Check your own skin monthly for new moles, sores that don’t heal, or patches that are red, scaly, or growing. Early detection of skin cancer is highly curable.
Do steroids increase cancer risk with TNF inhibitors?
Yes. Taking more than 7.5 mg of prednisone daily (or equivalent) while on a TNF inhibitor is linked to worse cancer outcomes and higher cancer-related death rates. Steroids add another layer of immunosuppression. Your doctor should aim to taper you off steroids as soon as your disease is under control.
What Comes Next?
If you’re considering a TNF inhibitor, ask your doctor for the latest data on your specific condition. If you’re already on one, make sure your skin checks are scheduled. If you’ve had cancer, don’t assume you’re automatically off-limits-get a second opinion. The goal isn’t to avoid treatment. It’s to use it wisely.
For millions, TNF inhibitors are the bridge back to life. The risk of cancer isn’t zero. But it’s not the monster we’ve been told it is. It’s a number. A manageable one. And with the right care, you can live well-with or without the drug.

9 Comments
Olivia Goolsby
December 28, 2025 AT 04:21Okay, but have you ever stopped to think that Big Pharma is using TNF inhibitors as a Trojan horse to get people hooked on lifelong immunosuppression so they can sell more cancer drugs later? The FDA’s black box warning? That’s just window dressing. They know the truth: TNF blockers don’t just increase cancer risk-they create a fertile breeding ground for it. And don’t get me started on the $6,000 monthly price tag-this isn’t medicine, it’s a corporate extortion racket disguised as a miracle cure. They want you dependent. They want you scared. They want you to keep coming back. And they’re winning.
Alex Lopez
December 29, 2025 AT 00:15While I appreciate the emotional weight of this post, I must respectfully note that the data presented is both nuanced and reassuring. The 30% increased risk of non-melanoma skin cancer is statistically significant but clinically modest-especially when weighed against the proven reduction in systemic inflammation, which independently elevates cardiovascular and oncologic risk. Moreover, the protopathic bias observed in early studies has been thoroughly addressed in longitudinal cohort analyses. For context: untreated RA carries a 1.5–2x higher lymphoma risk than TNF inhibitor use. So while vigilance (e.g., biannual dermatology visits) is prudent, fear is not evidence-based. 😊
John Barron
December 30, 2025 AT 23:47Let me drop some science on you 🧬. A 2023 Nature Genetics paper identified 12 SNPs that predict lymphoma susceptibility in TNF-inhibitor users with 89% accuracy. If you're on Humira and haven't gotten a polygenic risk score? You're flying blind. Also-etanercept isn't 'safer.' It's just less likely to bind to transmembrane TNF, which reduces skin penetration. But here's the kicker: the real cancer driver isn't the drug-it's the IL-6/STAT3 pathway that gets upregulated in chronic inflammation. So if your CRP is still high on biologics, you're still at risk. And yes, I'm a rheumatology researcher. I've seen 47 patients on TNF inhibitors. 3 got skin cancer. All caught early. Because they checked their skin. 🧴🩺
Anna Weitz
December 31, 2025 AT 22:27People act like cancer is this random monster but it's just your body screaming because it's been poisoned by modern life-processed food, plastic, pollution, stress. TNF inhibitors? They're just the latest scapegoat. The real villain is your diet. Your sleep. Your phone. Your fear. You think a shot fixes anything? Nah. You're just numbing the symptom while the root rots. Wake up. Your immune system isn't broken-it's betrayed. And no drug will fix that. Only truth. Only presence. Only silence.
Jane Lucas
January 2, 2026 AT 09:15i just started humira last month and honestly i was terrified but after reading this i feel way calmer. i check my skin every week now and my derm said my moles look fine. i dont smoke and i dropped my prednisone to 5mg. i just wanna be able to play with my niece without crying from pain. thats worth a little extra vigilance.
Elizabeth Alvarez
January 2, 2026 AT 10:52Have you heard about the secret studies? The ones the FDA buried? They found that TNF inhibitors cause DNA fragmentation in lymphocytes within 30 days of use. But they didn't publish it because the drug companies own the journals. And now they're pushing genetic testing to scare people into thinking it's 'personal risk' instead of systemic poisoning. They're turning patients into guinea pigs with 'personalized medicine' while the real data gets buried under layers of corporate jargon. You think your skin check saves you? It's a distraction. The poison is already in your blood. You just don't know it yet.
Miriam Piro
January 2, 2026 AT 14:10What if the real cancer isn't in your cells… but in your belief system? We’ve been conditioned to fear death so much that we’ll surrender our autonomy to a pill that promises safety but steals our vitality. TNF inhibitors don’t cure inflammation-they commodify it. You trade your body’s natural wisdom for a monthly injection and a false sense of control. And then you’re told to check your skin like it’s a chore, not a sacred ritual. You’re not managing risk-you’re surrendering to a system that profits from your fear. The cure isn’t in a vial. It’s in listening. In stillness. In letting your body heal… without interference.
Todd Scott
January 3, 2026 AT 16:19As someone who’s lived with Crohn’s for 22 years and been on biologics since 2010, I’ve watched this debate evolve. The fear around cancer risk was real in the early 2000s-but the data has matured. In my cohort of 112 patients tracked over 15 years, we had 3 cases of non-melanoma skin cancer (all caught early) and zero lymphomas. Meanwhile, 5 developed severe joint damage from uncontrolled disease. The trade-off isn’t theoretical-it’s lived. And here’s what I tell new patients: don’t let fear of a 0.02% annual increase in lymphoma risk blind you to the 70% chance this drug will get you back to your kid’s soccer game. The real risk? Not trying.
Andrew Gurung
January 5, 2026 AT 02:28Wow. Just… wow. This post reads like a pharmaceutical pamphlet written by someone who’s never felt the weight of a life interrupted. You call this ‘informed choice’? It’s corporate gaslighting wrapped in a data bow. And now you want us to get ‘skin checks’ like it’s a spa day? Please. If you’re on Humira and you think you’re ‘managing risk,’ you’re just another cog in the machine. Real healing doesn’t come from injections. It comes from radical lifestyle change. From fasting. From grounding. From rejecting the sick system that sold you this lie. You’re not sick-you’re spiritually compromised. And no drug can fix that.