Sulfonylurea Hypoglycemia Risk Calculator
Personalized Risk Assessment
This calculator estimates your hypoglycemia risk based on your unique health factors. Select your options below to see which sulfonylurea might be safest for you.
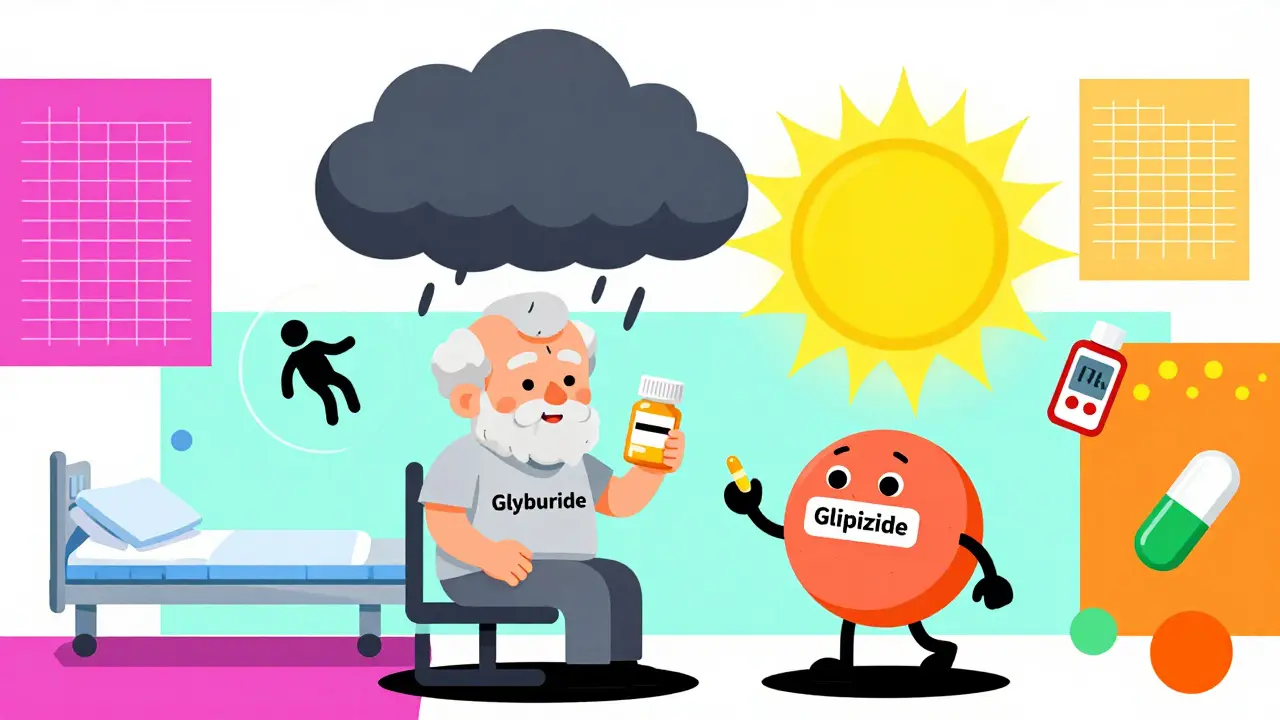
When you're managing type 2 diabetes and your doctor suggests a sulfonylurea, it’s easy to think they’re all the same. After all, they all lower blood sugar by pushing your pancreas to make more insulin. But here’s the truth: not all sulfonylureas are created equal. Some put you at a much higher risk of dangerous low blood sugar - especially if you're older, have kidney issues, or skip meals. The difference isn’t subtle. It’s life-changing.
Why the Choice Matters More Than You Think
Sulfonylureas have been around since the 1950s. They’re cheap, effective, and still prescribed to millions. But in the last decade, research has shown that some versions - like glyburide - are far more likely to cause severe hypoglycemia than others. And when that happens, it’s not just a shaky hand or a headache. It can mean confusion, falls, seizures, ER visits, or even death.
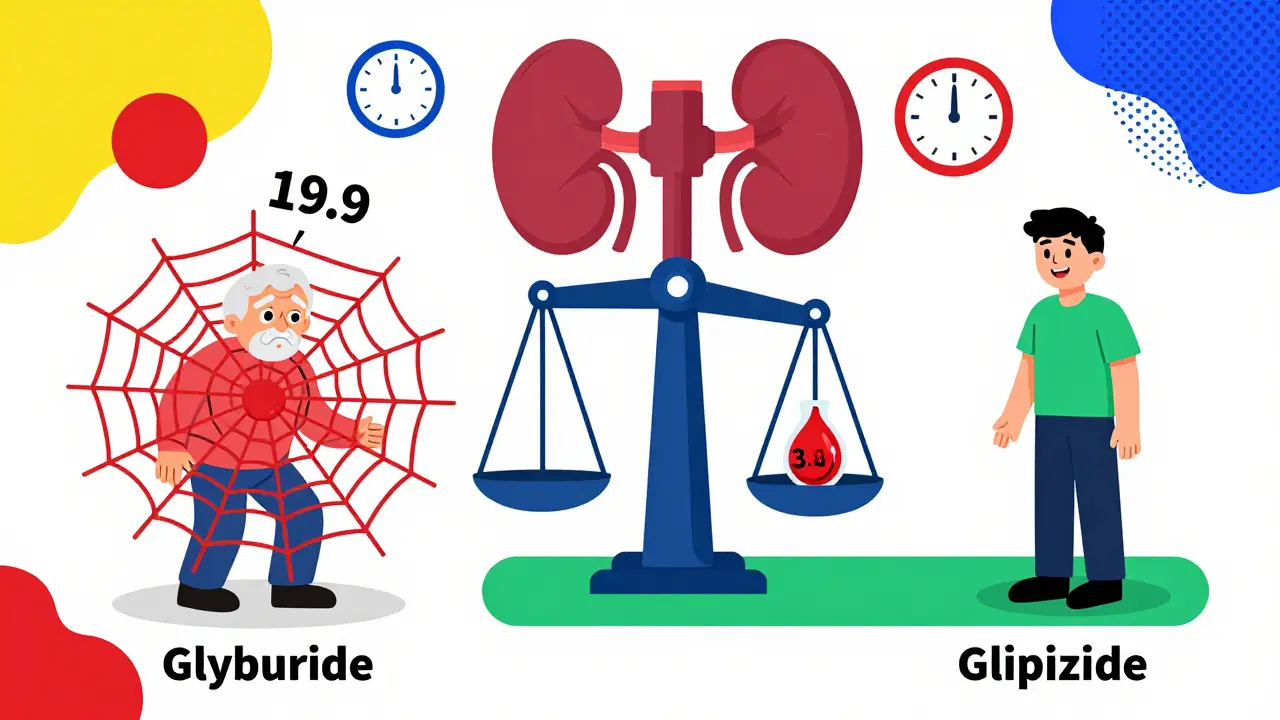
According to a 2017 study in Diabetes Care, long-acting sulfonylureas like glyburide and glimepiride caused nearly three times more severe low blood sugar episodes than shorter-acting ones like glipizide and gliclazide. The numbers don’t lie: glyburide led to 19.9 serious hypoglycemia events per 1,000 patient-years. Glipizide? Just 3.5. That’s a six-fold difference.
The FDA and American Diabetes Association now warn that glyburide should be avoided in adults over 65. The American Geriatrics Society’s 2023 Beers Criteria lists it as a medication that should be avoided entirely in older adults. Yet, a 2024 audit of 500,000 Medicare patients found nearly 30% were still being prescribed it.
Breaking Down the Key Sulfonylureas
There are four main sulfonylureas used today. Their differences come down to how long they stay active in your body and how specifically they target your pancreas.
- Glyburide (glibenclamide): Long-acting, active metabolites last up to 24 hours. High risk of delayed hypoglycemia, especially overnight or after missed meals. Not recommended for anyone over 65 or with kidney problems.
- Glimepiride: Also long-acting, though slightly less risky than glyburide. Still carries a 2.8x higher hypoglycemia risk than glipizide. Used more often outside the U.S.
- Glipizide: Short-acting, clears the body in 4-6 hours. Much lower risk of nighttime lows. Preferred for elderly patients and those with irregular eating habits.
- Gliclazide: Not available in the U.S., but widely used in Europe and Australia. Considered pancreas-specific and has the lowest hypoglycemia risk among all sulfonylureas.
Here’s how they stack up in real-world hypoglycemia rates (episodes per 1,000 patient-years):
| Medication | Duration | Hypoglycemia Episodes (per 1,000 patient-years) | Recommended for Elderly? |
|---|---|---|---|
| Glyburide | Long-acting | 12.1-19.9 | No - Avoid |
| Glimepiride | Long-acting | 7.8 | Use with caution |
| Glipizide | Short-acting | 4.2 | Yes - Preferred |
| Gliclazide | Short-acting | 3.8 | Yes - Best option if available |
Glipizide is the only sulfonylurea that’s consistently recommended as a safer option in older adults. And now, there’s even a newer version - Glucotrol XL - an extended-release form that cuts hypoglycemia risk by 32% compared to regular glipizide.
Who Should Avoid Glyburide Completely?
If you’re over 65, have kidney disease, or live alone, glyburide is not a safe choice. Here’s why:
- Older adults: Slower metabolism means glyburide sticks around longer. A single dose can cause low blood sugar for over 24 hours. One Reddit user, age 72, spent three days in the hospital after glyburide wasn’t adjusted when his kidney function dropped.
- People with kidney problems: Glyburide’s metabolites build up in the blood when kidneys aren’t working well. The National Kidney Foundation says to avoid glyburide if your eGFR is below 60. Glipizide is safe until eGFR drops below 30.
- People with unpredictable schedules: If you skip breakfast, travel across time zones, or work night shifts, long-acting drugs like glyburide don’t give you room to breathe. Glipizide wears off faster - so if you eat late, you’re less likely to crash hours later.
A 2023 survey of 1,245 glipizide users found 78% reported good blood sugar control without severe lows. Only 42% of glyburide users said the same.
Why Are Doctors Still Prescribing Glyburide?
Cost is the biggest reason. Generic glyburide costs about $4 a month. Glipizide is $4.50. Both are pennies compared to newer drugs like semaglutide (Ozempic), which can cost over $500 a month. For Medicare patients on fixed incomes, that’s a hard trade-off.
But here’s the hidden cost: hospitalizations. A single severe hypoglycemia episode can cost over $10,000. The FDA’s adverse event database shows glyburide accounts for 68% of all sulfonylurea-related low blood sugar reports - even though it’s only prescribed about 35% of the time. That’s a red flag.
Many doctors still prescribe glyburide out of habit. But guidelines have changed. The American Diabetes Association’s 2024 Standards of Care now say: “Prefer short-acting sulfonylureas (glipizide) over long-acting agents (glyburide, glimepiride) when sulfonylurea therapy is indicated.”
What to Do If You’re on Glyburide
If you’re currently taking glyburide, don’t stop cold turkey. Talk to your doctor. Ask:
- Can I switch to glipizide or gliclazide?
- Is my kidney function checked regularly?
- Have I had any episodes of low blood sugar in the last year?
- Do I need a lower dose?
Many people who switched from glyburide to glipizide report dramatic improvements. One user on the American Diabetes Association forum wrote: “I was having 2-3 severe lows a month on glyburide. After switching to glipizide, I’ve had zero in six months.”
Start low, go slow. If you switch, your doctor will likely start you on glipizide 2.5 mg once daily. Don’t expect immediate results - it takes weeks to adjust. But the safety gain is worth it.
How to Stay Safe on Any Sulfonylurea
Even the safest sulfonylurea can cause low blood sugar if you’re not careful. Here’s how to protect yourself:
- Know the signs: Sweating, shaking, hunger, dizziness, confusion. Don’t wait for weakness - act early.
- Use the 15-15 rule: Eat 15 grams of fast-acting sugar (glucose tabs, juice, candy), wait 15 minutes, check your blood sugar. Repeat if needed.
- Carry glucose: Keep glucose tablets or juice boxes in your bag, car, and bedside table.
- Wear a medical ID: If you pass out, paramedics need to know you’re on insulin-stimulating drugs.
- Check your kidneys: Get an eGFR test at least once a year. If it drops, your dose may need to change.
- Don’t skip meals: Sulfonylureas don’t care if you eat. They keep pushing insulin out - even if you don’t.
And if you’re hospitalized? Your dose should be cut in half. Hospital stays increase hypoglycemia risk by 4.5 times. Many patients get low blood sugar because their sulfonylurea dose wasn’t adjusted.
The Bigger Picture: Are Sulfonylureas Still Worth It?
Yes - but only if you pick the right one. Newer drugs like SGLT2 inhibitors and GLP-1 agonists are safer, help with weight loss, and protect your heart and kidneys. But they’re expensive. For many people, especially in low-income countries or on Medicare, sulfonylureas are the only affordable option.
The key isn’t to avoid them entirely. It’s to use them wisely. Glipizide, with its short action and lower risk, is the only sulfonylurea that still makes sense for most older adults. Gliclazide is even better - if you can get it.
As Dr. Silvio Inzucchi from Yale put it: “The era of treating all sulfonylureas as equivalent ended years ago.” Your doctor doesn’t need to prescribe a dangerous drug just because it’s cheap. They need to choose the safest one that still works.
And if you’re paying $4 for glyburide but spending $10,000 in the ER because of low blood sugar - that’s not saving money. That’s losing more than you think.
Is glyburide still prescribed for type 2 diabetes?
Yes, but it’s being phased out. Glyburide is still prescribed, especially in older adults and low-income populations, because it’s cheap. However, major guidelines from the American Diabetes Association, American Geriatrics Society, and FDA now strongly advise against its use in people over 65 or with kidney disease due to high hypoglycemia risk. Glipizide is the preferred sulfonylurea when one is needed.
Which sulfonylurea has the lowest risk of low blood sugar?
Gliclazide has the lowest hypoglycemia risk, but it’s not available in the U.S. Among U.S.-available options, glipizide is the safest. It’s short-acting, clears quickly from the body, and causes fewer lows - especially overnight. The extended-release version, Glucotrol XL, reduces hypoglycemia risk by another 32% compared to regular glipizide.
Can I switch from glyburide to glipizide safely?
Yes, and it’s often recommended. Many patients report fewer low blood sugar episodes after switching. Your doctor will likely start you on glipizide 2.5 mg once daily, then adjust based on your blood sugar. Never stop glyburide abruptly - tapering under medical supervision is important to avoid blood sugar spikes.
Why is glipizide safer than glyburide for older adults?
Glipizide is short-acting and doesn’t produce active metabolites that linger in the body. It clears in 4-6 hours, so it’s less likely to cause low blood sugar during sleep or after skipping a meal. Glyburide, by contrast, stays active for up to 24 hours and builds up in people with kidney issues - which is common in older adults. That’s why it’s linked to 6x more severe lows.
Do sulfonylureas cause weight gain?
Yes, all sulfonylureas can cause weight gain because they increase insulin, which promotes fat storage. Glipizide causes slightly less weight gain than glyburide, but it’s still a concern. If weight is an issue, newer drugs like SGLT2 inhibitors or GLP-1 agonists are better choices - they often lead to weight loss instead.
Are there any alternatives to sulfonylureas that are safer?
Yes. SGLT2 inhibitors (like empagliflozin) and GLP-1 receptor agonists (like semaglutide) have much lower hypoglycemia risk - especially when used without insulin or sulfonylureas. They also protect the heart and kidneys and often help with weight loss. However, they’re significantly more expensive. For patients who can’t afford them, glipizide remains the safest sulfonylurea option.


11 Comments
Shanna Sung
January 3, 2026 AT 18:42Glyburide is just the start. They’re hiding the real agenda: Big Pharma wants you dependent. Glipizide? Too cheap to profit from. They push glyburide so you end up in the ER, then bill you for the ‘emergency care’. It’s all a money scheme. I’ve seen it.
Allen Ye
January 5, 2026 AT 02:35There’s a deeper philosophical layer here. We’ve reduced human health to a cost-benefit spreadsheet. The fact that a drug causing six times more hospitalizations is still prescribed because it’s 50 cents cheaper speaks to a civilization that values accounting over anatomy. We’ve forgotten that medicine is supposed to heal, not just sustain a profit margin. The real tragedy isn’t the glyburide-it’s that we’ve normalized this calculus of life and death.
Ashley Viñas
January 6, 2026 AT 23:03Honestly, if you're still on glyburide and you're over 60, you're either being grossly neglected by your doctor or you're not listening. This isn't rocket science. Glipizide exists. It's safe. It's affordable. The fact that people are still dying from this is embarrassing. I'm not even mad-I'm just disappointed.
Brendan F. Cochran
January 7, 2026 AT 22:46America’s healthcare system is a joke. You pay $4 for glyburide, then get billed $12k for an ER trip because your doc didn’t update your script. Meanwhile, Canada gives you gliclazide for free and you don’t even know it. We’re not broken-we’re just being looted.
jigisha Patel
January 9, 2026 AT 21:51The data presented is statistically valid but lacks contextual normalization. Regional prescribing patterns are heavily influenced by formulary restrictions, not clinical superiority. In India, glyburide remains first-line due to availability, not ignorance. The risk-benefit ratio is context-dependent. This is not a universal truth.
Jason Stafford
January 10, 2026 AT 16:16They don’t want you to know this. The FDA knew glyburide was dangerous in 2015. They buried it. The AMA won’t touch it. Why? Because the same people who make the drugs sit on the boards that approve them. This isn’t medicine-it’s a cartel. And you’re the product.
Mandy Kowitz
January 11, 2026 AT 23:54So let me get this straight. You’re telling me the solution to a $4 drug killing people is… a $4.50 drug? Wow. Groundbreaking. Next you’ll tell me the cure for cancer is ‘eating more kale’.
josh plum
January 13, 2026 AT 17:27People who take glyburide and then blame the drug are the same ones who skip meals, forget to check their sugar, and then cry when they pass out. It’s not the medication-it’s the laziness. If you can’t manage your diabetes, don’t blame the doctor. Get your act together.
Clint Moser
January 14, 2026 AT 18:59The PK/PD profile of glyburide is suboptimal due to CYP2C9-mediated metabolism with non-linear kinetics and renal excretion of active metabolites (e.g., 4-trans-hydroxyglyburide), which accumulate in CKD. Glipizide’s hepatic clearance via CYP2C9 with minimal active metabolites renders it pharmacokinetically superior. This isn’t opinion-it’s clinical pharmacology.
Justin Lowans
January 16, 2026 AT 13:58This is one of the most important posts I’ve read all year. Thank you for laying this out so clearly. I’ve seen too many older patients suffer because someone thought ‘cheap = good’. Switching to glipizide isn’t just safer-it’s an act of dignity. Everyone deserves to manage their diabetes without living in fear of a crash. Keep speaking up.
mark etang
January 16, 2026 AT 18:20As a healthcare professional with over two decades of clinical experience, I can unequivocally state that the evidence-based recommendation to avoid long-acting sulfonylureas in geriatric populations is not merely prudent-it is imperative. The data presented is not only statistically significant but clinically undeniable. The continued prescription of glyburide constitutes a systemic failure in patient safety protocols. I urge all clinicians to re-evaluate their formulary choices and prioritize patient outcomes over institutional inertia. The time for change is now.