Imagine taking your medication every day like clockwork-until one morning, you just can’t bring yourself to do it. Not because you forgot. Not because you’re lazy. But because the voice in your head says, ‘It’s not helping. I’m fine without it. Why keep taking this?’ That’s not weakness. That’s the illness talking. And it’s why medication adherence in mental health is one of the biggest, quietest crises in modern medicine.
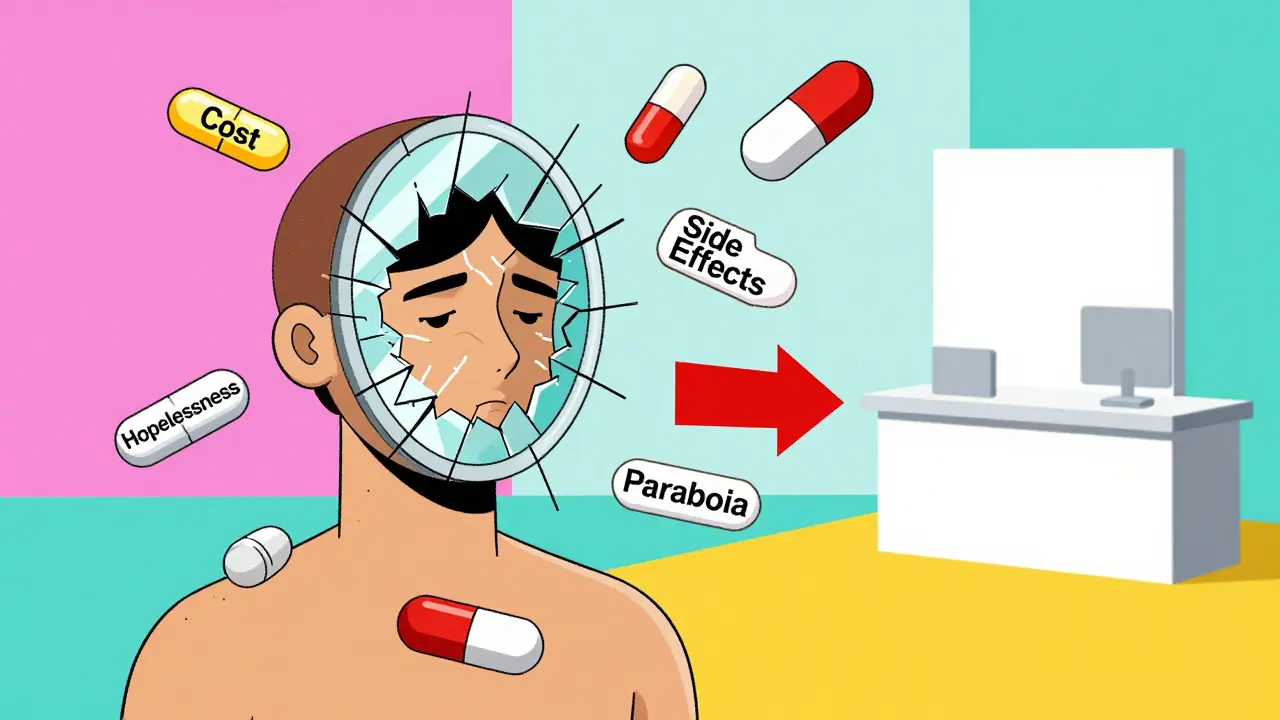
Half of people with schizophrenia don’t take their meds as prescribed. Up to 60% of those with bipolar disorder or major depression miss doses. And it’s not just about willpower. It’s about side effects, cost, stigma, confusion, and the cruel irony that the very symptoms you’re trying to treat-like hopelessness or paranoia-make it harder to stick with treatment. The result? More hospital visits, more relapses, more lost years. The CDC calls it an ‘invisible epidemic.’ And it’s costing the U.S. system up to $300 billion a year in avoidable care.
Why Do People Stop Taking Their Mental Health Meds?
People don’t stop because they’re careless. They stop because something feels worse than taking the pill.
Some feel the meds dull their emotions too much. Others can’t afford them-$500 a month for an antipsychotic isn’t rare. Some don’t believe they’re sick. Others are scared of long-term effects. A study from Columbia University found that patients with depression were 40% less likely to take any medication at all, even for other conditions like high blood pressure, because they felt worthless or saw no point.
And then there’s the dosing. Taking four pills a day? That’s a full-time job. One patient on Reddit said, “I’d take my meds if I didn’t have to remember five different times a day. I’m already forgetting to eat.” Simplifying regimens-from three times daily to once-boosts adherence from 52% to 87%, according to NAMI. Yet 73% of patients say their doctor never even asked if they could switch to a simpler schedule.
Homeless individuals? Their adherence rate drops to 26%. Why? No fridge to store meds. No phone to set reminders. No stable place to sleep, let alone a routine. The system isn’t broken for them-it was never built for them.
What Actually Improves Adherence? (The Real Solutions)
Not apps. Not posters. Not yelling at patients to “just take your pills.” The data shows what works-and what doesn’t.
Pharmacist-led care is the most powerful tool we have. When a pharmacist works side-by-side with a psychiatrist, reviews meds, explains side effects in plain language, and checks in weekly, adherence jumps by up to 40%. In Kaiser Permanente’s Northern California program, hospitalizations dropped 18% in just 90 days. The savings? About $1,200 per patient annually. And it’s not magic-it’s accountability, education, and access.
One patient in Melbourne told me, “My pharmacist knew my meds better than my GP. She noticed I’d stopped taking the mood stabilizer. She called me. Didn’t judge. Just asked, ‘What’s going on?’” That’s the difference.
Long-acting injectables (LAIs) are changing the game. For schizophrenia, oral meds have a 56% adherence rate. LAIs? 87%. One shot every two weeks. No daily pills. No hiding them. No forgetting. The FDA highlighted this in 2024, and CMS now tracks it as a quality metric. Yet only 1 in 5 eligible patients get offered this option. Why? Stigma. Misconceptions. Fear of injections. But the data doesn’t lie: if you can’t swallow a pill reliably, an injection might be the most humane choice.
Cost matters more than you think. A 2025 study found that when patients got free medication through a pharmacy program, adherence jumped from 38% to 82% in six months. Insurance won’t cover it? Copays are too high? That’s not a patient problem-it’s a system failure. Programs that offer $0 copays for psychiatric meds see immediate, measurable gains in adherence.
Personalized action plans beat generic advice. Telling someone, “Take your meds,” doesn’t help. Asking, “What makes it hard for you to take your meds on Tuesdays?” does. A 2025 Frontiers in Psychiatry trial showed that patients who co-created a daily routine with their pharmacist-linking pill-taking to brushing teeth or eating breakfast-had 142% better adherence than those getting standard care.
What Doesn’t Work (And Why)
Most digital apps? They’re nice, but they don’t move the needle much. A study showed only a 1.8% increase in adherence for statins using apps. For mental health meds? Even less. Why? Because loneliness, shame, and confusion aren’t fixed by a notification. If you’re too depressed to open your phone, an app won’t save you.
Therapy alone? Helpful, but not enough. Cognitive behavioral therapy can improve insight, but if the pill costs $400 and you’re sleeping on a park bench, therapy won’t pay for it.
Shaming patients? Catastrophic. “You’re not trying hard enough” is the worst thing you can say. It deepens the belief that you’re broken, not sick.
And here’s the kicker: most clinics still don’t track adherence at all. They assume you’re taking your meds. CMS now requires clinics to measure Proportion of Days Covered (PDC) for schizophrenia patients. But only 32% of community mental health centers are doing it right. If you’re not measuring it, you’re not treating it.
The System Is Failing-But Change Is Happening
It’s not all bleak. Real progress is being made, quietly, in pockets of the system.
UnitedHealthcare now ties 12% of provider payments to whether patients hit the 80% adherence target for antipsychotics. That’s a financial incentive to care. CMS is raising the weight of adherence in Star Ratings from 10% to 15% by 2027. That means health plans will compete to keep patients on meds.
AI is coming. Epic Systems is building real-time adherence alerts into their 2026 EHR. If a patient hasn’t picked up a script in 30 days, the system flags it. The doctor gets a nudge. The pharmacist gets a call. It’s not surveillance-it’s support.
And in Australia, some pharmacies now offer free medication reviews for people on multiple psychiatric drugs. No appointment needed. Just walk in. That’s the kind of low-barrier access that works.

What You Can Do-If You’re a Patient, Family Member, or Clinician
Here’s the practical stuff. No fluff.
- If you’re a patient: Ask your doctor, “Can I switch to a once-daily version?” or “Is there a long-acting shot?” Don’t wait for them to bring it up. Bring it up yourself.
- If you’re a family member: Don’t nag. Ask, “What’s the hardest part about taking your meds?” Then listen. Offer to help set a phone alarm. Or pick up the script. Small things matter.
- If you’re a clinician: Stop assuming adherence. Measure it. Use PDC. Talk about cost. Offer LAIs. Partner with a pharmacist. If your clinic doesn’t have one, push for it.
- If you’re a policymaker or insurer: Cover LAIs. Eliminate copays for psychiatric meds. Pay pharmacists to do medication therapy management. It saves money. It saves lives.
Adherence isn’t about compliance. It’s about connection. When someone feels heard, seen, and supported-not judged-they’re far more likely to take the next pill. And the next. And the next.
It’s Not About Willpower. It’s About Design.
We wouldn’t expect someone with a broken leg to walk 10 miles a day without crutches. Yet we expect someone with schizophrenia to remember four pills a day while battling delusions, fatigue, and poverty-and then blame them when they fail.
It’s time to stop asking people to be perfect. Start designing systems that work for the broken, the tired, the scared, and the unheard.
Because medication adherence in mental health isn’t a patient problem. It’s a human problem. And it’s solvable.