Living with migraine isn’t just about having a bad headache. It’s about losing entire days - missing work, skipping family events, or lying in a dark room while your body feels like it’s under siege. For over a billion people worldwide, migraine is a neurological disorder that doesn’t go away with a nap or an ibuprofen. The good news? We now have more tools than ever to take control - not just to stop attacks, but to prevent them before they start.
What Makes Migraine Different From a Regular Headache?
Migraine isn’t a headache with extra symptoms. It’s a complex brain condition with its own diagnostic rules. According to the International Classification of Headache Disorders, 3rd Edition (ICHD-3), a true migraine attack lasts 4 to 72 hours and includes at least two of these features: pain on one side of the head, a pulsing quality, moderate to severe intensity, and worsening with movement. It’s also usually paired with nausea, sensitivity to light, or sensitivity to sound.
If you get visual disturbances - flashing lights, blind spots, zigzag lines - before the headache hits, that’s called migraine with aura. About 90% of aura cases involve vision changes. Less common but just as real: tingling in your hand or face, trouble speaking, or even temporary weakness. These symptoms build slowly over 5 to 60 minutes and fade before the pain starts.
Chronic migraine is diagnosed when you have headaches on 15 or more days per month for at least three months, with at least eight of those days meeting migraine criteria. That’s not occasional discomfort - that’s life interrupted nearly every day.
Preventive Treatments: Stopping Migraines Before They Start
Prevention is where the biggest shift in migraine care has happened. Instead of just treating pain after it hits, doctors now focus on reducing how often attacks occur - ideally by half or more. This isn’t about taking a pill every day just in case. It’s about targeting the biological roots of migraine.
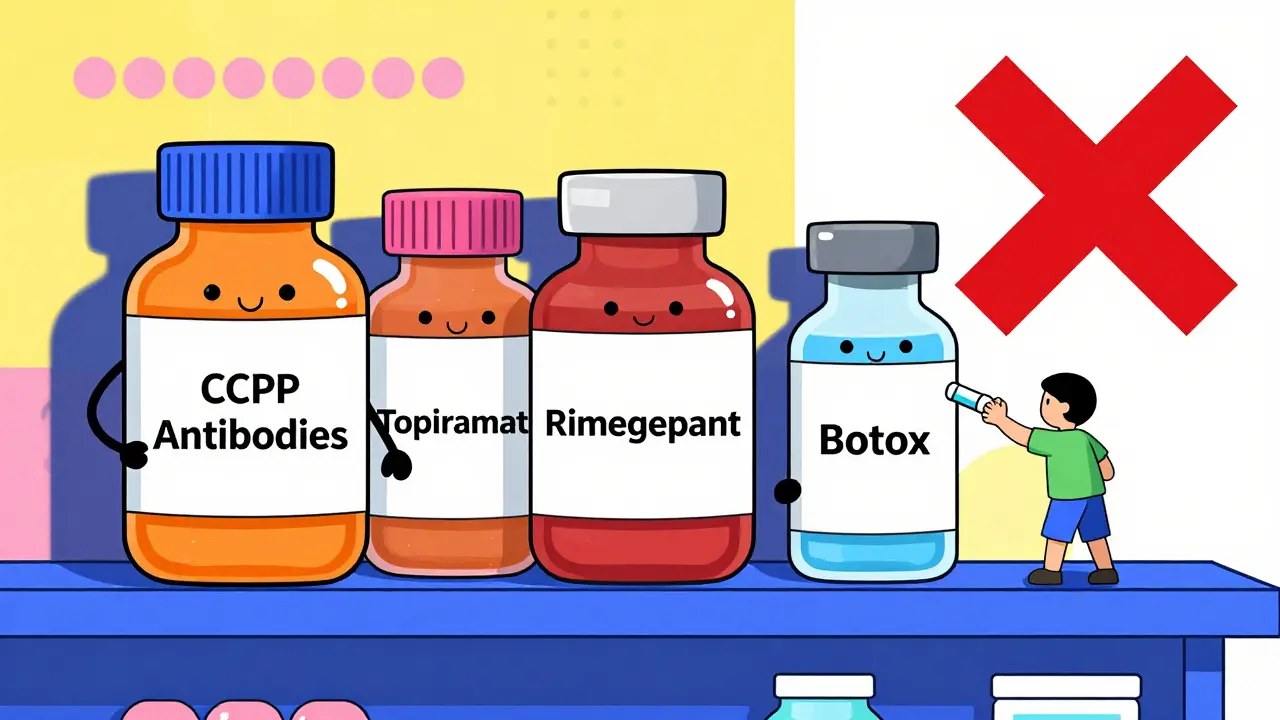
First-line medications include beta-blockers like propranolol and metoprolol, anticonvulsants like topiramate and valproate, and calcium channel blockers like verapamil. These have been around for years and work for about 50-60% of people. But they come with trade-offs. Topiramate can cause brain fog, memory lapses, or trouble finding words. About 55% of people stop taking it within six months because of side effects.
CGRP monoclonal antibodies changed everything in 2018. These are the first migraine-specific preventives. Drugs like erenumab, fremanezumab, galcanezumab, and eptinezumab block a protein called calcitonin gene-related peptide, which plays a key role in triggering migraine attacks. They’re given as monthly or quarterly injections or infusions. In clinical trials, 50-62% of patients cut their migraine days by at least half. Side effects? Usually mild - injection site reactions or constipation. Discontinuation rates are just 5-10%, compared to 15-30% with topiramate.
But here’s the catch: they cost $650 to $750 a month. Insurance often denies coverage. Only about 35% of eligible patients get them, according to JAMA Neurology in 2023. Prior authorization support from drug manufacturers helps - 85% of appeals succeed when guided properly.
Botox is another preventive option, but only for chronic migraine. It’s injected into 31-39 sites on the head and neck every 12 weeks. In the PREEMPT trials, patients saw an average of 8.4 fewer headache days per month - better than placebo by nearly two days.
Non-drug options are gaining traction. The Cefaly device is a headband that delivers mild electrical pulses to the supraorbital nerve. Used 20 minutes a day, it helped 38% of users reduce attacks by at least half in the ESPOUSE trial. The gammaCore device stimulates the vagus nerve with 90-second treatments three times a day. And mindfulness programs - eight weeks of meditation and breathing exercises - reduced headache frequency by 1.4 days per week in a 2022 JAMA Neurology study.
Acute Treatments: Stopping a Migraine in Its Tracks
When a migraine hits, speed matters. The sooner you treat it, the better the outcome. Experts recommend acting within 20 minutes of the first sign - whether it’s an aura, a dull throb, or a sudden wave of nausea.
Over-the-counter pain relievers like ibuprofen (400 mg) or naproxen (500-850 mg) work for mild attacks. They give you a 20-30% chance of being pain-free in two hours. Combination pills like Excedrin Migraine (aspirin, acetaminophen, caffeine) are slightly better - about 26% pain-free at two hours. But using these more than 10 days a month can trigger medication-overuse headaches. That’s when your body gets used to the medicine, and headaches become daily.
Triptans are the gold standard for moderate to severe attacks. There are seven types: sumatriptan, rizatriptan, eletriptan, zolmitriptan, almotriptan, frovatriptan, and naratriptan. They work by narrowing blood vessels in the brain and blocking pain pathways. In clinical studies, they give you a 30-50% chance of being pain-free in two hours. But they’re not safe for everyone. If you have heart disease, high blood pressure, or a history of stroke, you can’t use them.
Gepants like ubrogepant and rimegepant are newer. They block CGRP without affecting blood vessels, so they’re safe for people who can’t take triptans. Rimegepant is also approved for prevention. In trials, ubrogepant gave a 19.2% pain-free rate at two hours - better than placebo (11.8%). Users on Reddit report higher satisfaction with rimegepant than sumatriptan, citing fewer side effects.
Lasmiditan is a ditan - a different class that targets serotonin receptors in the brain without constricting blood vessels. It’s useful for those with cardiovascular risks. But it causes dizziness and sedation in up to 40% of users, so don’t drive after taking it.
Anti-nausea meds like metoclopramide or prochlorperazine are often given in emergency rooms. They don’t just calm the stomach - they help the migraine meds absorb better. In one study, metoclopramide relieved nausea in 70% of patients.
Stay away from opioids and barbiturates. The American Headache Society strongly advises against them. They don’t work better than other options, and they carry a high risk of addiction and medication-overuse headaches.
What Works Best Together?
Combining acute and preventive treatments gives the best results. The 2023 American Registry for Migraine Research tracked 5,217 patients and found that those using both approaches had a 62% success rate in cutting headache days by 50% or more. Those on just one type of treatment? Only 45%.
For example: someone on monthly fremanezumab (preventive) might keep a rimegepant tablet on hand for breakthrough attacks. Or a person using Cefaly daily might take an NSAID early if they feel a migraine coming on.
It’s not about stacking drugs. It’s about matching tools to your pattern. If you get migraines 15 days a month, prevention is essential. If you only get them once a month, you might just need a reliable acute treatment.
Triggers and Lifestyle: The Hidden Players
Medications aren’t the whole story. Triggers matter - and they’re different for everyone. A 2023 survey of 1,247 migraine patients found:
- 89% said stress was a trigger
- 72% pointed to weather changes
- 65% cited sleep disruption
- 58% named certain foods (aged cheese, processed meats, MSG, alcohol)
Keeping a headache diary - digital or paper - helps spot patterns. The 2022 Headache Log app showed 40% better adherence than paper logs. You don’t need to be perfect. Just note: date, time, symptoms, what you ate, how much you slept, stress level, and what you took.
Prodrome symptoms - the warning signs that come 24 to 48 hours before the headache - are often ignored. Mood changes, food cravings, neck stiffness, or excessive yawning can be early clues. If you recognize them, you can start treatment earlier and stop the migraine before it fully develops.
What Doesn’t Work - And What to Avoid
Not all treatments are created equal. Many people try supplements like riboflavin, magnesium, or coenzyme Q10. Some studies show modest benefit, but they’re not reliable for everyone. Don’t skip proven treatments just because you’re hoping for a natural fix.
Medication-overuse headache is a silent trap. It happens when you use acute meds - even OTC ones - more than 10 days a month. The headache gets worse, not better. Detox can take months. One Reddit user wrote: “Using Excedrin 15 days a month led to daily headaches. I needed six months to recover.”
Some people avoid triptans because of chest tightness or drowsiness. Those are real side effects - experienced by 63% and 45% of users respectively. But they’re usually temporary. Talk to your doctor before giving up. There are seven types - one might work better than another.
Topiramate’s cognitive side effects are brutal for many. Word-finding trouble, memory lapses - 68% report them. If you’re a writer, teacher, or speaker, this can be unbearable. Dose titration - slowly increasing the dose over weeks - cuts discontinuation rates from 55% to 28%.
What’s Coming Next?
The field is moving fast. In 2023, the FDA approved atogepant - the first oral CGRP blocker that works for both prevention and acute treatment. Clinical trials showed 41% of users cut monthly migraine days by half.
Non-invasive vagus nerve stimulators are getting smaller and smarter. The gammaCore Sapphire II is expected to show better results in late 2024. Digital therapeutics like the Relieve app, which uses behavioral therapy, reduced headache days by 32% in a 2023 trial.
Looking ahead, experts predict personalized treatment by 2030. Imagine a wearable that detects changes in your heart rate or skin conductance hours before a migraine. Add your genetic profile and trigger history, and your phone could tell you: “Take your gepant now. Avoid caffeine. Go to bed early.”
For now, the best approach is simple: understand your migraine, track your patterns, and work with a specialist - even if it’s just once. Primary care providers trained in migraine management now have an 87% accuracy rate in diagnosis after short courses. You don’t need to wait years to get help.
Frequently Asked Questions
Can migraine be cured?
No, migraine cannot be cured - but it can be managed effectively. Many people reduce attacks by 75% or more with the right combination of prevention, acute treatment, and lifestyle adjustments. Some even reach a point where they rarely need medication. The goal isn’t perfection - it’s regaining control of your life.
Are CGRP inhibitors worth the cost?
For chronic migraine sufferers who’ve tried at least three other preventives without success, yes. They’re more effective and better tolerated than older drugs like topiramate. While they cost $650-$750 a month, manufacturer assistance programs and prior authorization support often lower out-of-pocket costs. If you’re missing work or family time due to headaches, the cost of not treating it may be higher.
Why do I get migraines even when I avoid all triggers?
Migraine is a neurological disorder with a strong genetic component. Triggers like stress or weather changes can set off an attack, but they don’t cause the underlying condition. Even if you avoid every known trigger, your brain may still be primed to misfire. That’s why prevention meds are often necessary - they lower your brain’s overall sensitivity to triggers.
Is it safe to take triptans with blood pressure medication?
It depends. Triptans can raise blood pressure slightly and constrict blood vessels, so they’re not recommended if you have uncontrolled hypertension, heart disease, or a history of stroke. If you’re on blood pressure meds and have no cardiovascular issues, your doctor may still approve them after a careful review. Always get checked before starting.
How long does it take for preventive meds to work?
It varies. Beta-blockers and anticonvulsants usually take 4 to 8 weeks to reach full effect. CGRP antibodies can show results in the first month - some patients notice fewer attacks after the first injection. Botox takes about 10 to 14 days after the first treatment. Don’t give up if you don’t see results right away. Give it time, and track your progress.
Can children get migraines?
Yes. Migraine affects about 10% of school-age children and up to 28% of teens. In kids, attacks are often shorter, and pain may be on both sides of the head. Nausea and vomiting are common. Diagnosis is clinical - no scans needed. Treatment includes age-appropriate doses of NSAIDs or triptans, plus behavioral strategies like sleep hygiene and stress management.
Next Steps
If you’re struggling with migraine, start here: write down your last three attacks. When did they start? What were you doing? What helped? What made it worse? Bring that to your doctor. Ask about CGRP inhibitors if you’ve tried at least two preventives without success. If you’re using OTC meds more than 10 days a month, talk about medication-overuse headache. You don’t have to live like this. The tools are here - you just need to find the right combination.


10 Comments
Sara Stinnett
December 30, 2025 AT 23:03Let me be the first to say this: if you're still taking topiramate and calling it 'management,' you're not managing anything-you're just tolerating cognitive fog like it's a lifestyle choice. CGRP inhibitors aren't expensive-they're *corrective*. The fact that insurance still treats them like luxury goods is a moral failure disguised as policy. Your brain isn't a broken toaster you fix with duct tape and caffeine.
linda permata sari
January 1, 2026 AT 10:26OMG I just cried reading this. 🥹 I had my first migraine at 14, thought it was just 'bad stress,' and spent 17 years being told I was 'dramatic.' Now I'm on fremanezumab and I just hugged my kid for the first time in years without flinching. This isn't medicine-it's a second chance. Thank you for writing this like someone who actually *lives* it.
Brandon Boyd
January 3, 2026 AT 01:52Listen-you don’t need to wait for a miracle drug. Start with Cefaly. It’s $300 once, and you use it while scrolling TikTok. I went from 12 migraine days a month to 4 in six weeks. No pills. No needles. Just a headband that buzzes like a tiny alien massage. And yes, it looks ridiculous-but so does crying in the grocery store because the lights are too bright. Do the weird thing. It works.
Branden Temew
January 4, 2026 AT 23:24So we’ve replaced one kind of chemical dependency-with another. We’ve traded ibuprofen for $700 injections and called it ‘progress.’ Meanwhile, the real problem-the societal pressure to perform while your nervous system is screaming-isn’t even on the table. We treat the symptom like it’s the disease, and call it innovation. Brilliant. Truly. 🎩
Frank SSS
January 5, 2026 AT 19:06I’ve tried everything. Botox, topiramate, triptans, magnesium, yoga, cold showers, essential oils, a $200 ‘migraine pillow’-nothing stuck. Then I stopped fighting it. I started saying ‘no’ to parties, naps became sacred, and I stopped apologizing for needing darkness. The meds help-but the real win was learning to be selfish with my energy. No guilt. No explanations. Just… rest.
Paul Huppert
January 7, 2026 AT 01:52Anyone else notice how the article mentions Reddit users but doesn’t link to r/migraine? That sub is pure gold-real stories, no fluff. I’ve been on rimegepant for 3 months. Pain-free 80% of the time. My only complaint? It’s not covered by my plan. I’m saving up. Worth it.
Hanna Spittel
January 8, 2026 AT 09:20gotta be honest-cgrp inhibitors are just a big pharma scam to make us pay for 'premium' headaches 😒 also, did you know the FDA approved them because a lobbyist's wife had migraines? 🤫 #conspiracy
Brady K.
January 9, 2026 AT 10:58Let’s talk about the elephant in the room: the fact that 89% of migraine patients cite stress as a trigger… and yet we’re still asking them to ‘manage’ it with a $750/month injection instead of fixing the culture that burns people out. You can’t pharmacologically fix capitalism. But hey-let’s keep selling pills while the world keeps spinning into chaos. #Neurocapitalism
John Chapman
January 9, 2026 AT 17:34Y’all are overthinking this. If you’re having more than 8 headache days a month, you need a specialist. Not your PCP. Not a wellness coach. A headache doc. They exist. They’re not magic. But they know the difference between a cluster and a migraine. Go. Now. Your future self will hug you.
Marilyn Ferrera
January 9, 2026 AT 21:28For anyone considering gepants: rimegepant is the only one that doesn’t make me feel like I’ve been hit by a truck. Ubrogepant? Dizzy for hours. Rimegepant? Clear-headed. Also-yes, it’s approved for prevention AND acute. One pill. Two uses. Why isn’t everyone talking about this?!