Anticoagulation for PVT: What You Need to Know About Treatment and Risks
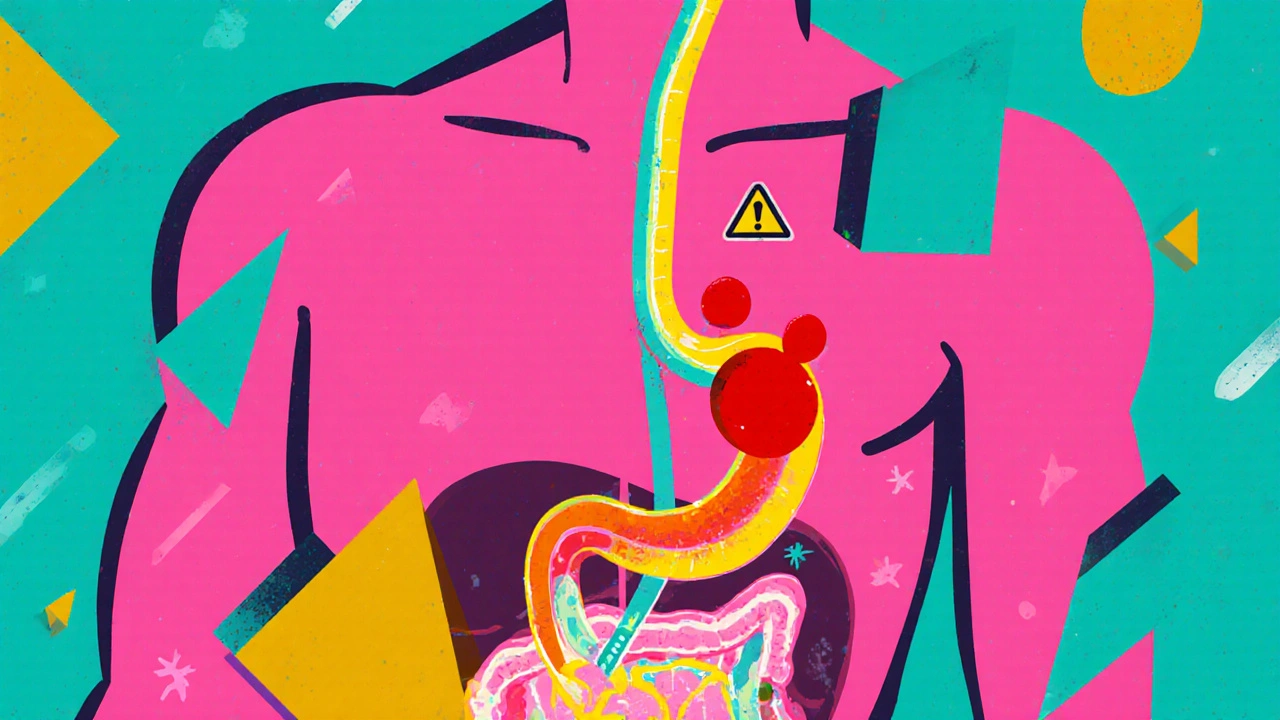
When a blood clot forms in the portal vein, the main blood vessel carrying blood from the intestines to the liver. Also known as portal vein thrombosis, it can block blood flow and lead to serious liver damage. This isn’t just a rare condition—it shows up in people with liver cirrhosis, cancer, or after abdominal surgery. Left untreated, it can trigger life-threatening complications like portal hypertension or intestinal ischemia. That’s where anticoagulation, the medical use of blood-thinning drugs to stop clots from growing or spreading. Also known as anticoagulant therapy, it’s often the first line of defense comes in.
Not everyone with PVT needs anticoagulation, but for many, it’s life-changing. Studies show that people with cirrhosis and PVT who get anticoagulants like warfarin or direct oral anticoagulants (DOACs) have better survival rates and lower risk of clot extension. But it’s not simple. The liver is already struggling in these patients, so dosing becomes tricky. Too little, and the clot keeps growing. Too much, and you risk bleeding—especially in the gut, which is already fragile. That’s why doctors look at the whole picture: liver function, platelet count, and whether the clot is new or old. Some patients get short-term treatment; others need it for months or even years. And it’s not just about the drug—it’s about monitoring. Regular blood tests, tracking symptoms like abdominal pain or swelling, and knowing when to adjust treatment make all the difference.
Anticoagulation for PVT also connects to other conditions you might see in these patients. For example, if someone has portal hypertension, high pressure in the portal vein system that often leads to enlarged veins and bleeding risk, anticoagulants can help prevent new clots from making it worse. Or if they’re dealing with hepatic encephalopathy, a brain disorder caused by liver failure, some blood thinners may interact with their other meds. And if smoking is part of their history—something we know from other posts increases clot risk—quitting becomes part of the treatment plan too.
You won’t find a one-size-fits-all answer here. That’s why the posts below cover real cases: how anticoagulants are chosen, what side effects to expect, how liver disease changes the game, and what happens when treatment fails. Whether you’re a patient, a caregiver, or just trying to understand the science, these guides give you the facts without the fluff. What works for one person might not work for another—and these articles show you why.
Portal Vein Thrombosis: Diagnosis and Anticoagulation Explained
Portal vein thrombosis is a serious but treatable condition. Early diagnosis and anticoagulation improve survival and recanalization rates. Learn how to diagnose PVT and choose the right blood thinner based on liver function and bleeding risk.
© 2026. All rights reserved.