Disseminated Candidiasis: Causes, Risks, and Treatments
When dealing with Disseminated Candidiasis, a severe, widespread infection where Candida fungi move beyond the bloodstream to infect multiple organs. Also known as systemic candidiasis, it usually starts as candidemia, the presence of Candida in the blood, and can quickly involve the kidneys, liver, eyes, or brain. The rise of Candida auris, a drug‑resistant species, has made the condition even harder to control, while growing antifungal resistance forces clinicians to rethink standard treatment plans.
Why does this infection spread so aggressively? First, many patients in intensive care units have weakened immune systems, central lines, or receive broad‑spectrum antibiotics that wipe out helpful bacteria. Those hospital environments become breeding grounds for fungal spores, and when a catheter or IV line gets contaminated, Candida can slip into the bloodstream. Once inside, the fungus exploits the body’s weakened defenses and travels to distant sites – a process captured in the semantic triple: Disseminated Candidiasis encompasses multi‑organ invasion. Another triple links the setting to the pathogen: Hospital exposure influences Candida auris emergence. Finally, treatment decisions hinge on the third triple: Antifungal resistance requires alternative drug regimens. Together, these connections explain why clinicians stress early detection and aggressive therapy.
Key Points to Watch
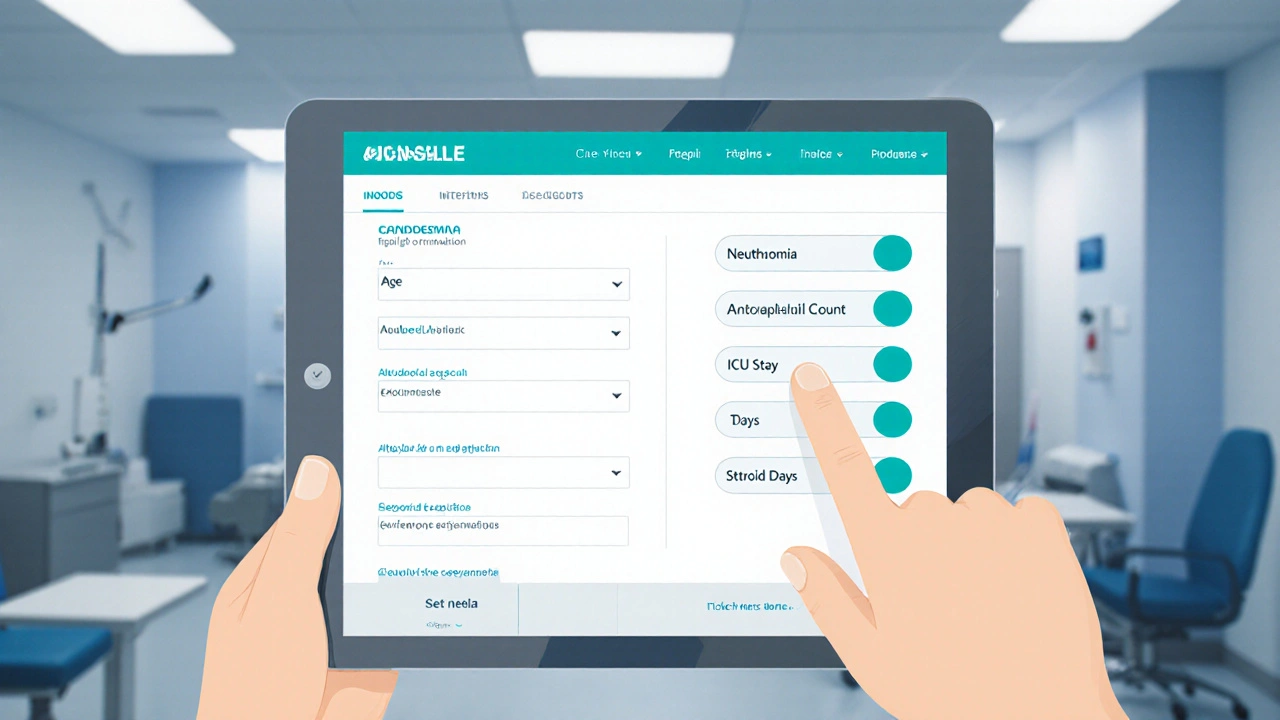
Patients most at risk include those with neutropenia, recent abdominal surgery, or prolonged use of central venous catheters. Blood tests that flag positive cultures for Candida are the first red flag, but because the infection can hide in organs, imaging studies (CT or MRI) become essential to map its spread. When Candida auris is identified, labs often report high minimum inhibitory concentrations, signaling that standard azoles or echinocandins may fail. In such cases, clinicians may turn to newer agents like ibrexafungerp or amphotericin B formulations, illustrating the triple: Candida auris influences treatment choice.
Prevention strategies focus on strict hand hygiene, careful catheter management, and judicious antibiotic use. Some hospitals now employ routine fungal surveillance cultures in high‑risk units, aiming to catch colonization before it turns into candidemia and, ultimately, disseminated disease. Education of staff and patients about early symptoms—persistent fever, unexplained abdominal pain, or visual changes—helps shorten the window between infection onset and therapy.
Below you’ll find a collection of articles that dive deeper into each aspect of disseminated candidiasis. From the latest data on Candida auris outbreaks to practical guides on choosing the right antifungal regimen, the posts are organized to give you both the big picture and the detailed steps you need to manage this serious infection effectively.
Candidemia, Disseminated Candida Infections & Opportunistic Infections: How They’re Linked
Explore how candidemia, disseminated Candida infections, and other opportunistic infections are linked, their shared risk factors, diagnosis, treatment, and prevention strategies.
© 2026. All rights reserved.