GI Bleed Stabilization: What Works, What Doesn’t, and How to Stay Safe
When someone has a GI bleed stabilization, the immediate medical response to stop bleeding in the digestive tract and prevent shock. Also known as gastrointestinal bleeding management, it’s not just about stopping blood loss—it’s about keeping organs alive long enough for the real fix to happen. This isn’t a slow-progressing issue. A major GI bleed can drop blood pressure in minutes, and every second counts. The goal? Keep oxygen flowing to the brain and heart while doctors figure out where the leak is and how to seal it.
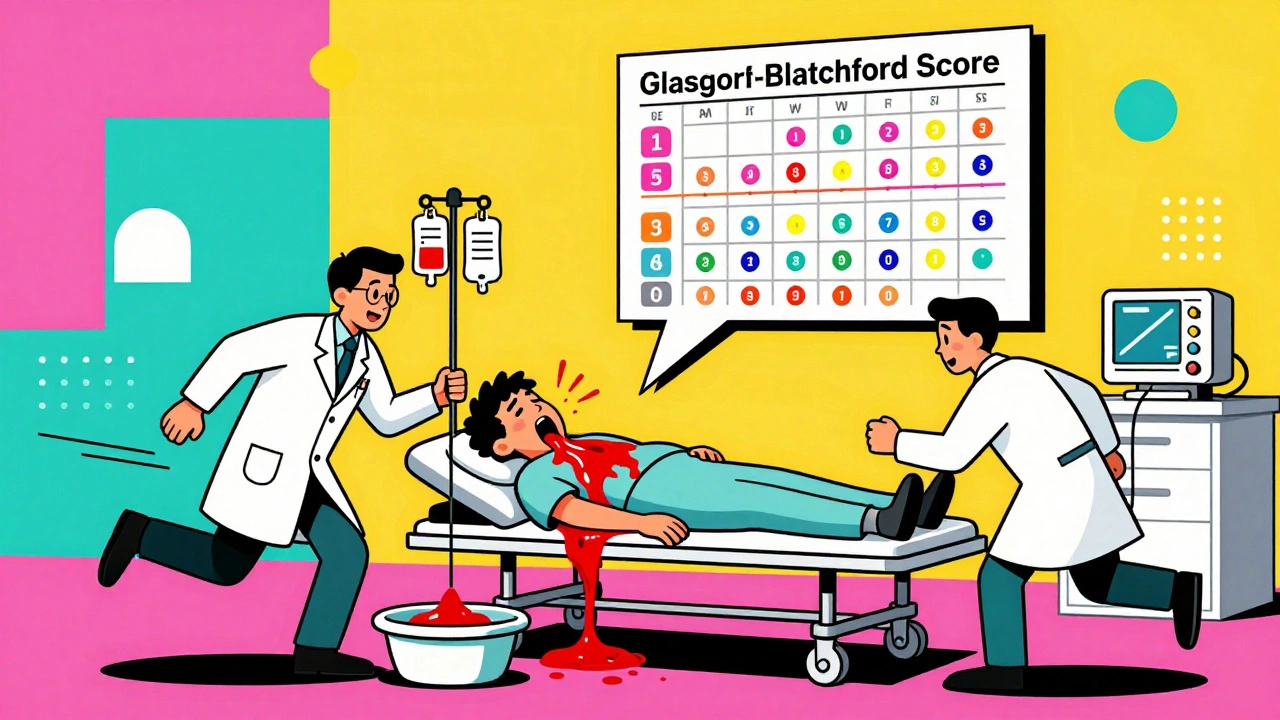
What happens first? Fluid resuscitation, the rapid delivery of IV fluids to replace lost blood volume and maintain circulation. This isn’t just water—it’s saline, sometimes blood products, and sometimes specific solutions to stabilize clotting. You can’t fix a bleed if the body’s already in shock. Then comes endoscopy, a procedure using a camera-equipped tube to find and treat the bleeding site directly. It’s not just diagnostic—it’s therapeutic. Doctors can burn, clip, or inject the spot causing the leak right then and there. Delay endoscopy, and the risk of rebleeding jumps by nearly 50%.
Medications play a supporting role. Proton pump inhibitors, drugs that shut down stomach acid production to help ulcers heal are often started immediately, even before the source is confirmed. Why? Because many GI bleeds come from ulcers, and acid makes them worse. Antibiotics are used too—if the bleed is linked to liver disease, infection risk spikes. And no, aspirin or NSAIDs aren’t just discouraged—they’re stopped cold. Even a single pill can restart bleeding.
Not all bleeds are the same. Upper GI bleeds—like from stomach ulcers or swollen veins in the esophagus—come with vomiting blood or black, tarry stools. Lower GI bleeds show up as bright red blood in stool, often from diverticula or colon polyps. The approach changes slightly, but the core goal stays the same: stabilize fast, find the source fast, stop it fast. Patients with cirrhosis or on blood thinners? They’re at higher risk, and their stabilization plan needs extra care.
What doesn’t work? Guessing. Waiting for symptoms to get worse. Assuming it’s just indigestion. Too many people delay care because they think it’ll pass. It won’t. And hospitals aren’t just throwing drugs at the problem—they’re using real-time monitoring, blood tests, and imaging to guide every move. The best outcomes come when stabilization starts within the first hour.
Below, you’ll find real-world insights from posts that cover the drugs, risks, and medical decisions tied to GI bleeding—from how anticoagulants complicate things, to why certain pain meds can trigger a bleed, to what happens after the emergency is over. This isn’t theory. These are the facts that save lives.
Upper GI Bleeding: Ulcers, Varices, and Stabilization
Upper GI bleeding is a life-threatening emergency caused by ulcers, varices, or other damage to the upper digestive tract. Learn the signs, causes, and life-saving stabilization steps used in modern medicine.
© 2026. All rights reserved.