PVT Diagnosis: Understanding Portal Vein Thrombosis and Related Conditions
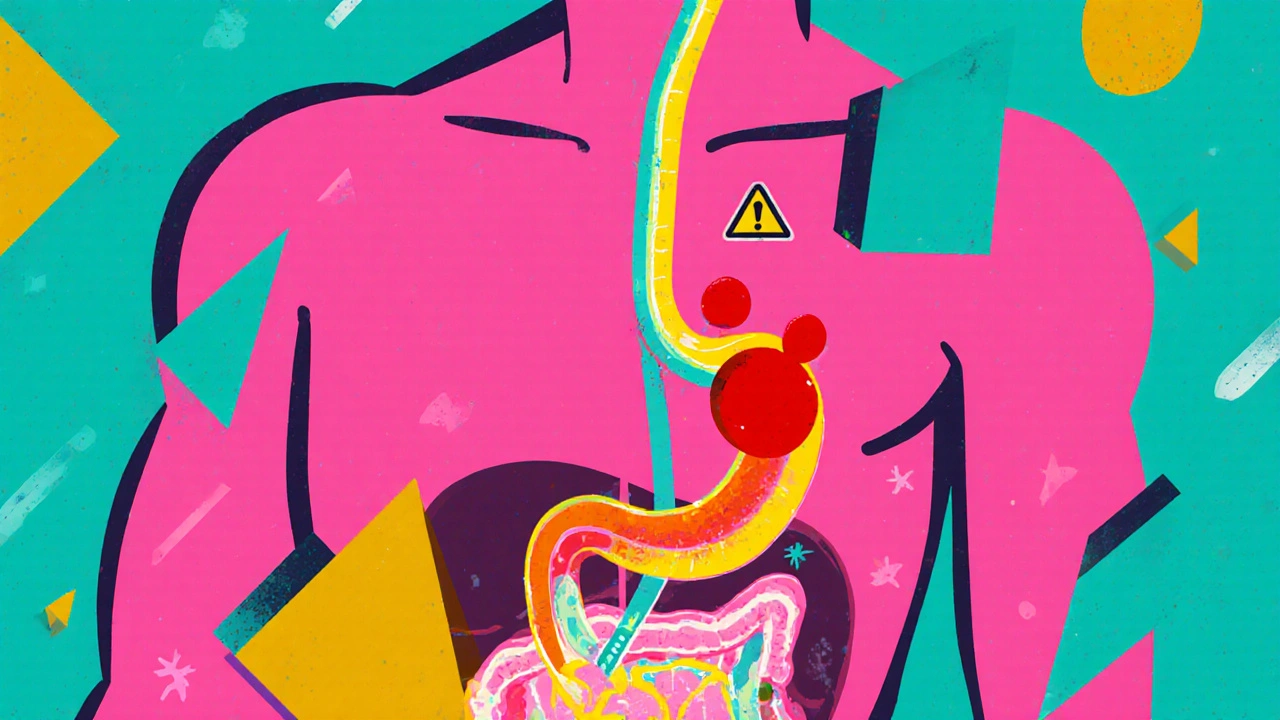
When doctors talk about PVT diagnosis, the process of detecting a blood clot in the portal vein that carries blood from the intestines to the liver. Also known as portal vein thrombosis, it’s not just a random clot—it’s often a sign of something deeper, like cirrhosis, liver cancer, or an infection in the abdomen. This isn’t something you feel right away. Many people don’t know they have it until they’re tested for another issue, like unexplained belly pain, swelling, or abnormal liver tests.
PVT diagnosis usually starts with imaging. Ultrasound is the first go-to because it’s quick, safe, and shows blood flow clearly. If the clot isn’t obvious, doctors may move to CT or MRI scans to get a sharper picture. But finding the clot is only half the battle. The real question is: why did it form? That’s where things get personal. People with chronic liver disease, especially cirrhosis, are at higher risk. So are those who’ve had recent abdominal surgery, suffer from inflammatory bowel disease, or have inherited blood clotting disorders. Even some cancers, like pancreatic or colorectal, can trigger it. It’s not just about the liver—it’s about the whole system.
And it’s not just the clot itself that’s dangerous. When the portal vein gets blocked, pressure builds up in the veins around the stomach and intestines. That can lead to dangerous bleeding, fluid buildup in the belly (ascites), or even brain fog from toxins the liver can’t filter out (hepatic encephalopathy). That’s why PVT diagnosis isn’t a one-and-done test—it’s a gateway to understanding your overall liver health. You might be looking at a clot, but what you’re really seeing is your body’s warning signal.
Some people think if they don’t have jaundice or vomiting, they’re fine. But PVT can sneak up quietly. That’s why doctors now check for it more often in patients with unexplained abdominal symptoms or worsening liver function. The good news? When caught early, blood thinners can stop it from getting worse. In some cases, the clot even clears on its own. But if it’s ignored, it can lead to long-term damage, increased risk of liver failure, or complications that need surgery.
What you’ll find below are real, practical guides from people who’ve been there. From how PVT connects to cirrhosis complications and liver cancer risks, to how medications like anticoagulants are chosen, and what symptoms to watch for after diagnosis. These aren’t textbook summaries—they’re clear, no-fluff breakdowns from patients and doctors who’ve dealt with this firsthand. Whether you’re trying to understand a recent diagnosis or helping someone else navigate it, this collection gives you the facts without the jargon.
Portal Vein Thrombosis: Diagnosis and Anticoagulation Explained
Portal vein thrombosis is a serious but treatable condition. Early diagnosis and anticoagulation improve survival and recanalization rates. Learn how to diagnose PVT and choose the right blood thinner based on liver function and bleeding risk.
© 2026. All rights reserved.