When your lungs feel tight and every breath takes effort, asthma isn’t just a diagnosis-it’s a daily reality. Around 300 million people live with it worldwide, and while it’s common, many still don’t understand the difference between an inhaler and an oral pill when it comes to managing it. This isn’t about fancy medical jargon. It’s about knowing what actually works, what doesn’t, and why your doctor might push one treatment over another.
What Kind of Asthma Do You Have?
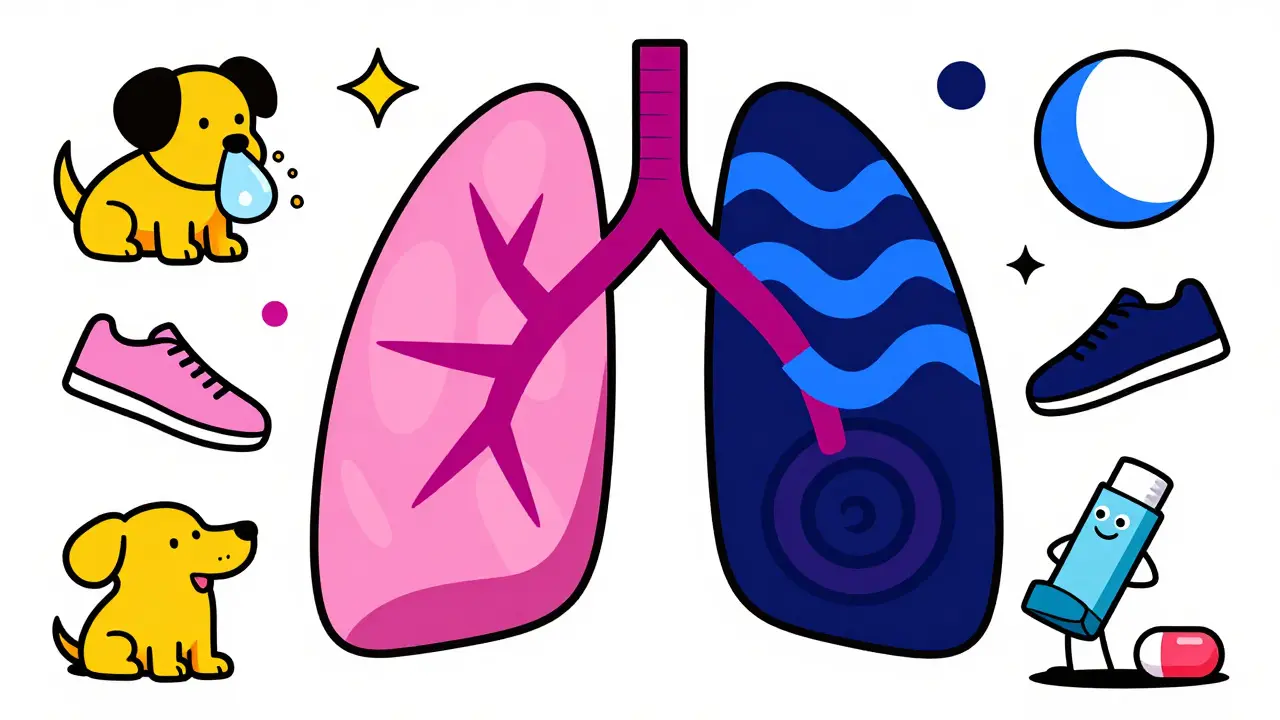
Not all asthma is the same. Two people can have the same symptoms-wheezing, coughing, chest tightness-but for totally different reasons. That’s why doctors don’t just treat asthma; they treat your type of asthma. Allergic asthma is the most common. It flares up when you breathe in pollen, dust mites, or pet dander. If your symptoms get worse in spring or after hugging your dog, this is likely yours. Then there’s exercise-induced asthma, where running, even on a cool morning, can trigger a coughing fit. Nighttime asthma hits when you’re lying down, often because of dust mites in your pillow or changes in your body’s natural rhythms. Some types are rarer but serious. Aspirin-induced asthma means even a simple painkiller like ibuprofen can shut your airways. Occupational asthma shows up only at work-maybe from cleaning chemicals, sawdust, or fumes. And then there’s steroid-resistant asthma, where standard inhalers barely help, no matter how hard you try. Doctors now talk about asthma in terms of endotypes-the hidden biology behind the symptoms. Eosinophilic asthma, for example, means your body makes too many of a certain white blood cell that causes swelling in your lungs. Neutrophilic asthma involves different cells. And some people have no clear inflammation at all. Knowing which endotype you have can change everything. It’s why a drug like mepolizumab, an injectable biologic, works wonders for some but does nothing for others.What Makes Your Asthma Flare Up?
Triggers aren’t just annoying-they’re dangerous. And they’re personal. What sets off one person’s asthma might leave another completely fine. For allergic asthma, it’s usually airborne stuff: pollen in spring, mold in damp basements, or pet hair clinging to clothes. But triggers don’t stop there. Cold air? A common one. A sudden drop in temperature can make your airways contract like a clenched fist. Smoke-whether from cigarettes, fireplaces, or wildfires-is another major culprit. Even strong perfumes or cleaning sprays can do it. For some, it’s not what they breathe in-it’s what they take. NSAIDs like ibuprofen or aspirin can cause severe reactions in people with aspirin-exacerbated respiratory disease. This isn’t just a side effect. It’s a full-blown asthma attack. And then there’s the silent trigger: stress. Emotional highs and lows don’t just affect your mood-they can tighten your airways. A 2023 study showed that people who reported high stress levels had twice as many asthma flare-ups, even when their medication use stayed the same. The key? Track your triggers. Keep a simple log: what you were doing, where you were, what you ate or breathed, and how bad your symptoms got. Over time, patterns emerge. You might notice your asthma spikes every time you clean the bathroom. Or after eating takeout with MSG. That’s not coincidence. That’s data you can use.Inhalers: The First Line of Defense
If you’ve got asthma, chances are your doctor started you on an inhaler. And for good reason. Inhalers deliver medication straight to your lungs. That means less of it gets into your bloodstream, which cuts down on side effects. There are two main types: rescue inhalers and maintenance inhalers. Rescue inhalers, like albuterol, are your quick fix. They open your airways in minutes. You use them when you’re struggling to breathe. But they don’t fix the inflammation-that’s why they’re not for daily use. Maintenance inhalers are the long-term solution. Most contain inhaled corticosteroids (ICS), like fluticasone or budesonide. These reduce swelling in your airways over time. You take them every day, even when you feel fine. That’s the trick: prevention beats crisis. Combination inhalers, like Advair or Symbicort, mix a steroid with a long-acting bronchodilator. They’re the go-to for moderate to severe asthma. And now, for mild asthma, guidelines have shifted. Instead of using a rescue inhaler alone, doctors now recommend using a low-dose steroid inhaler (like budesonide-formoterol) only when needed. This cuts down on severe attacks by more than half, according to the 2022 SYGMA trials. But here’s the catch: most people use inhalers wrong. A 2023 study found 60-80% of users make at least one critical mistake. Maybe they don’t shake it first. Or they don’t hold their breath after inhaling. Or they don’t use a spacer-a plastic tube that helps the medicine reach your lungs instead of sticking to your throat. Spacers are cheap, easy, and life-changing. Especially for kids. If you’re not using one, you’re getting maybe half the dose you think you are.
Oral Medications: When Inhalers Aren’t Enough
Oral medications are the backup plan. They’re not your first choice. They’re your emergency tool. Oral corticosteroids like prednisone are powerful. They can stop a bad asthma attack in its tracks. But they come with a price. Take them for more than a few days, and you risk weight gain, mood swings, high blood sugar, bone thinning, and even cataracts. One study showed 68% of long-term users gained weight. Another found a 30-50% higher risk of fractures. That’s why doctors avoid them for daily use. If you’re on oral steroids more than twice a year, your asthma isn’t controlled. It’s time to rethink your treatment. Leukotriene modifiers like montelukast (Singulair) are oral pills taken daily. They’re less powerful than steroids but safer. They help with allergic asthma and exercise-induced symptoms. Some people use them alongside inhalers for extra control. But they’re not magic. Studies show they add about 15-20% more symptom relief-not enough to replace inhalers, but helpful as a sidekick. The real game-changer? Biologics. These are injectable drugs like mepolizumab or tezepelumab. They target specific parts of your immune system that drive inflammation. They’re not for everyone. Only for severe asthma that doesn’t respond to other treatments. But for those who qualify, they can slash attacks by 50-60%. One user on PatientsLikeMe said, “I went from two ER visits a year to zero. I didn’t even know I could feel this normal.”Why Inhalers Win-Most of the Time
Let’s cut through the noise. Inhalers are better. Not because they’re trendy. Because they work better and are safer. A 2022 study in the Journal of Allergy and Clinical Immunology found inhaled steroids cause 70% fewer side effects than oral ones. That’s not a small difference. That’s the difference between feeling okay and feeling sick from your own medicine. On Reddit’s asthma community, 78% of 1,245 users said they prefer inhalers. One wrote: “My inhaler takes 10 seconds. I feel better in 5 minutes. No mood swings. No weight gain.” Oral steroids? They’re the opposite. A 2023 survey of 2,500 severe asthma patients found 62% said oral steroids hurt their quality of life. Weight gain (87%), sleep problems (76%), and anxiety (68%) were the top complaints. Cost is another factor. Generic oral meds like montelukast cost $10-$30 a month. But brand-name inhalers? $300-$400 without insurance. That’s why 25% of U.S. asthma patients ration their inhalers-skipping doses to make them last. That’s dangerous. Skipping your daily inhaler is like skipping your car’s oil change. You don’t know it’s failing until it breaks down.
What’s Next for Asthma Treatment?
The future of asthma care is smarter, not just stronger. Smart inhalers with sensors now track when and how you use them. Devices like Propeller Health send alerts to your phone if you miss a dose or if your symptoms spike after being outside on a high-pollen day. A 2023 study in JAMA Internal Medicine found users improved adherence by 35% and cut flare-ups by 22% in just 12 months. Doctors are also moving toward personalized treatment. Instead of guessing which drug works, they’re testing your blood for biomarkers-like eosinophil levels-to match you with the right therapy. The NIH’s Precision Medicine Initiative aims to have these tools ready by 2026. Meanwhile, global access remains a huge problem. Eighty percent of asthma cases are in low- and middle-income countries. But only 30% of people there have reliable access to basic inhalers. This isn’t just a health issue. It’s a justice issue.What Should You Do Right Now?
If you have asthma, here’s what matters most:- Know your type. Is it allergic? Exercise-induced? Nighttime? That shapes your treatment.
- Track your triggers. Write them down. Look for patterns.
- Use your inhaler correctly. Get a spacer. Ask your pharmacist to watch you use it.
- Take your maintenance inhaler daily-even when you feel fine.
- Don’t rely on oral steroids. If you need them more than twice a year, talk to your doctor about stepping up your inhaler therapy.
- If you’re still struggling, ask about biologics. You might qualify.

2 Comments
Donna Macaranas
February 1, 2026 AT 20:59Just wanted to say this post made me feel seen. I’ve had allergic asthma since I was 5, and no one ever explained why my inhaler wasn’t a cure-all. Using a spacer changed everything. I used to think I was just bad at it-turns out, I was just never taught right.
Now I carry my spacer in my purse like a phone. No shame. My lungs thank me.
Also, yes to tracking triggers. I learned my asthma flares after eating takeout with MSG. Weird, but true.
Thanks for writing this like a human, not a textbook.
Naomi Walsh
February 3, 2026 AT 05:24How is this even considered ‘basic’? The post barely scratches the surface of endotypes. Did you mention TSLP or IL-33 pathways? No. Did you discuss the clinical relevance of FeNO testing? Not a word. And you call montelukast a ‘sidekick’? That’s amateurish terminology. Real clinicians use ‘leukotriene receptor antagonist’-not cartoon metaphors.
Also, citing Reddit polls as evidence? Pathetic. Where’s the meta-analysis? The Cochrane review? This reads like a blog written by a med student who just watched a YouTube video.