Living with a transplanted organ means more than just a second chance at life-it means living with a constant, complex balancing act. Every day, transplant recipients take a cocktail of powerful drugs to stop their immune system from attacking the new organ. But these lifesaving medications don’t just protect the transplant-they come with a long list of side effects and dangerous interactions that can reshape your health in ways you never expected.
Why Immunosuppressants Are Non-Negotiable
Your body sees a transplanted kidney, liver, or heart as an invader. Left unchecked, your immune system will destroy it. That’s why immunosuppressants are mandatory. Without them, graft rejection happens in days or weeks. Even today, with all the advances in medicine, the only exception is identical twins. For everyone else, lifelong immunosuppression is the rule, not the exception.The standard approach? A triple therapy combo: a calcineurin inhibitor (usually tacrolimus), an antimetabolite (often mycophenolate), and a corticosteroid like prednisone. This isn’t arbitrary. It’s based on decades of data. In the U.S., 92.4% of kidney transplant patients take tacrolimus because it outperforms cyclosporine-83% of grafts survive one year with tacrolimus versus 77% with cyclosporine, according to the ELITE-Symphony trial.
These drugs don’t just weaken your immune system randomly. They target specific pathways. Tacrolimus blocks T-cell activation by shutting down calcineurin. Mycophenolate stops immune cells from making DNA. Steroids dampen inflammation across the board. Each has a job. And each has consequences.
Drug Interactions: The Silent Threat
One of the most dangerous realities for transplant recipients isn’t the drugs themselves-it’s what they interact with. Most immunosuppressants, especially tacrolimus and cyclosporine, are broken down by an enzyme called CYP3A4. That’s the same enzyme that processes common medications like antibiotics, antifungals, and even some heart drugs.Take fluconazole, a common antifungal for yeast infections. It can spike tacrolimus levels by 50% to 200%. That’s not a small bump-it can cause kidney damage, tremors, seizures, or even death. On the flip side, rifampin, used for tuberculosis, can slash tacrolimus levels by 60-90%. That means your body might reject the transplant without you even realizing it.
Even over-the-counter stuff can be risky. St. John’s wort, a popular herbal remedy for depression, is a strong CYP3A4 inducer. It can make your immunosuppressants ineffective. Grapefruit juice? It blocks the same enzyme, raising drug levels dangerously. And don’t assume your pharmacist knows all the risks. Many aren’t trained in transplant-specific interactions. That’s why every new prescription-even for a simple headache-needs to be cleared by your transplant team.
Side Effects That Change Your Life
The side effects aren’t just inconvenient-they’re life-altering.Tacrolimus is linked to new-onset diabetes after transplantation (NODAT). About 20-30% of patients develop it. That means daily blood sugar checks, insulin shots, or oral meds. It’s not just about diet-it’s a direct effect of the drug on insulin-producing cells.
Mycophenolate causes gastrointestinal misery. Up to half of patients get diarrhea, nausea, or stomach pain. Some can’t tolerate it at all. That’s why some switch to azathioprine, but then they risk bone marrow suppression-low white blood cell counts that leave them vulnerable to infections.
Steroids like prednisone? They’re the most visible offenders. Weight gain isn’t just extra pounds-it’s 15 to 20 pounds in the first six months. Moon face. Buffalo hump. Thinning skin. Bruising easily. Mood swings. ‘Steroid rage’ is real. Many patients say they don’t recognize themselves in the mirror. And it’s not just cosmetic. Steroids cause osteoporosis. By year 10, 30-50% of transplant recipients have had a fracture. That’s five times the rate of the general population.
mTOR inhibitors like sirolimus are sometimes used to reduce kidney damage from tacrolimus. But they bring their own problems: mouth sores, high cholesterol, and slow wound healing. One patient on Reddit switched from tacrolimus to sirolimus after his kidney function dropped to 38 mL/min. His GFR climbed to 52-but now he gets mouth ulcers every month and needs a statin just to manage his cholesterol.

The Hidden Toll: Infections, Cancer, and Fatigue
Your immune system isn’t just protecting you from rejection-it’s fighting off everything else. With it turned down, you’re sitting ducks for infections. Pneumonia. Urinary tract infections. Even common colds can turn serious. The CDC says transplant patients are 100 times more likely to get certain HPV-related cancers. Skin cancer? About 23% of liver transplant recipients develop nonmelanoma skin cancer. That’s why annual dermatology checks are non-negotiable.And then there’s fatigue. Not just tired. Exhausted. A 2023 WebMD analysis found 72% of transplant recipients report chronic fatigue. Sleep is disrupted. Emotional stability is shaky. Depression and anxiety rates are higher than in the general population. It’s not ‘just in your head.’ It’s the drugs, the stress, the constant vigilance.
How to Manage It All
There’s no magic fix. But there are proven strategies.Medication adherence is the biggest predictor of graft survival. Yet 22% of late graft losses are due to patients skipping doses. That’s why many centers use electronic pill dispensers. One Cleveland Clinic study showed adherence jumped from 72% to 89% with them.
Therapeutic drug monitoring isn’t optional. Tacrolimus levels need checking every week for the first three months, then every two weeks, then monthly. Too low? Rejection risk. Too high? Kidney damage. The target range? 5-8 ng/mL in the first year. Anything outside that is dangerous.
Monitoring isn’t just blood tests. You need monthly CBCs to catch low blood counts. Quarterly lipid panels because cholesterol skyrockets. Biannual glucose tests because diabetes sneaks up. And annual skin checks.
Lifestyle adjustments matter. No raw fish. No undercooked eggs. No unpasteurized cheese. Listeria is deadly for you. Wear a mask in crowded places. Wash your hands constantly. Avoid gardening without gloves-fungus in soil can cause serious lung infections.
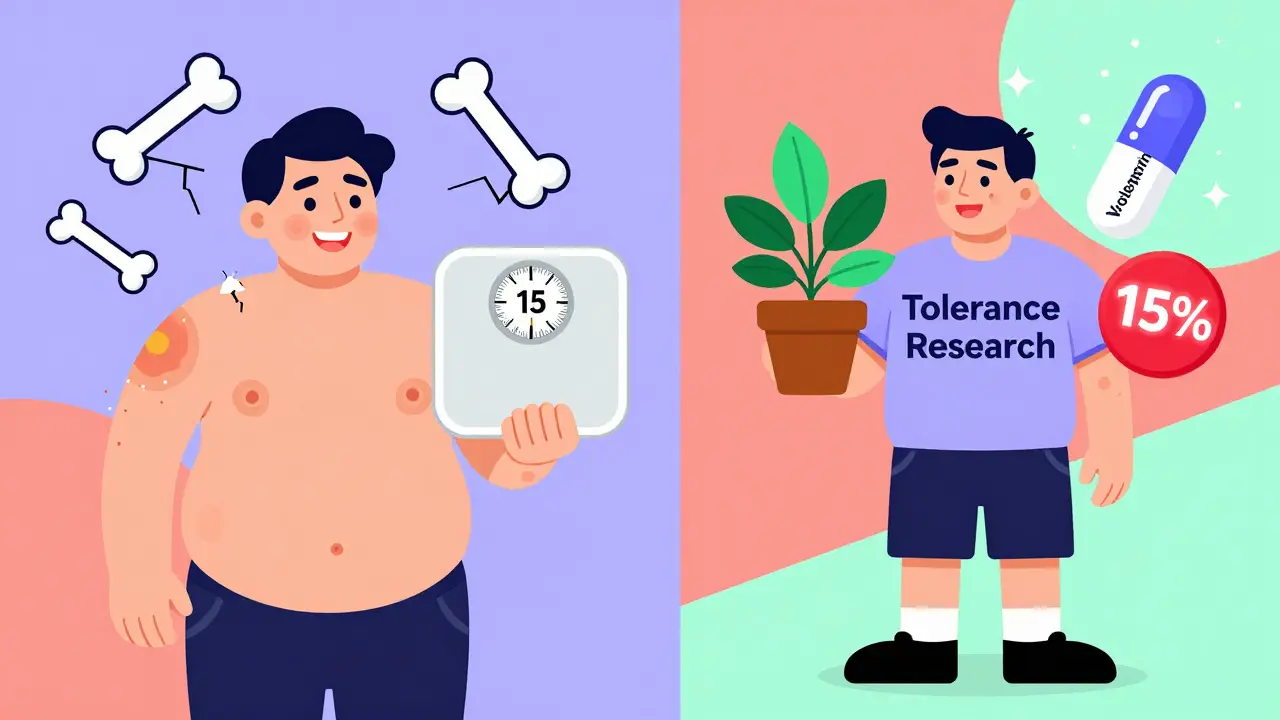
The Future: Toward Tolerance Without Drugs
The dream isn’t just better drugs-it’s no drugs at all. Researchers are working on immune tolerance. The ONE Study found that 15% of kidney transplant recipients treated with regulatory T-cell therapy could stop all immunosuppressants after two years. That’s groundbreaking.New drugs like voclosporin, approved by the FDA in 2023, show 24% less kidney toxicity than tacrolimus. Belatacept, a costimulation blocker, cuts cardiovascular deaths by 30% and cancer rates by 25%. But it causes more early rejection, so it’s not for everyone.
Most transplant centers now use early steroid withdrawal-stopping prednisone within 7-14 days for low-risk patients. That alone reduces weight gain, diabetes, and bone loss by 35-40%.
What Patients Really Say
On Reddit, u/KidneyWarrior writes: ‘I take 10 pills a day, three times a day. I have tremors so bad I can’t hold a coffee cup. My face looks swollen. I’m always cold. But I’m alive.’u/LiverSurvivor says: ‘I switched to sirolimus. My kidneys improved. But I got mouth ulcers every month. I needed statins. Was it worth it? Yes.’
These aren’t just stories. They’re data points. The National Kidney Foundation’s 2022 survey of 1,247 recipients found 41% said side effects hurt their quality of life more than the original illness.
But here’s the truth: the alternative is death. The 10-year survival rate for kidney transplant recipients is 65%. For people with kidney failure on dialysis? It’s 35%. The drugs are brutal. But they’re the price of life.
Transplant isn’t a cure. It’s a trade. You trade the risk of dying for the daily burden of managing side effects, interactions, and constant medical oversight. And you do it with the support of a team that knows every pill, every lab result, every warning sign.
Stay informed. Ask questions. Report every new symptom. Don’t assume it’s ‘just part of it.’ Some side effects are manageable. Some are signs of something worse. Your transplant team is there to help you navigate this-not just survive it, but live well within it.
Can I take over-the-counter painkillers after a transplant?
It depends. Acetaminophen (Tylenol) is generally safe at recommended doses. Avoid NSAIDs like ibuprofen or naproxen-they can damage your new kidney, especially if you’re on tacrolimus. Always check with your transplant team before taking anything, even aspirin or cold medicine.
Why do I need to live close to the transplant center?
For the first year, you need to be within 2 hours of the center. That’s because rejection or infection can happen suddenly and require emergency treatment-sometimes within hours. Blood tests, biopsies, and IV meds may be needed on short notice. 92% of U.S. transplant programs require this for safety.
Is it safe to get vaccinated after a transplant?
Yes-but not all vaccines are equally effective. You should get inactivated vaccines like flu, COVID-19, pneumonia, and shingles. Avoid live vaccines like MMR or nasal flu spray. Your immune system may not respond well, so timing matters. Talk to your team about when it’s safe to vaccinate after transplant.
Can I ever stop taking immunosuppressants?
For almost all patients, no. Immunosuppression is lifelong. The only exceptions are in rare research settings where immune tolerance has been induced-like in the ONE Study, where 15% of kidney recipients stopped drugs after two years. But this is experimental. Don’t consider stopping without your transplant team’s guidance-it can lead to immediate, irreversible rejection.
How do I know if my immunosuppressant levels are too high or too low?
You won’t feel it directly. Too high? Symptoms include tremors, headaches, high blood pressure, kidney problems, or seizures. Too low? You might develop fever, swelling, pain near the transplant, or decreased urine output-all signs of rejection. Regular blood tests are the only reliable way to know. Never adjust your dose based on how you feel.
Are there cheaper alternatives to brand-name immunosuppressants?
Yes. Generic cyclosporine (Gengraf) and mycophenolate (Myfortic) are available and cost 25-30% less. Tacrolimus generics are expected after its patent expires in 2025. But not all generics are equal. Some patients report differences in side effects or blood levels. Always work with your transplant team before switching to ensure stability.
What should I do if I miss a dose of my immunosuppressant?
If you miss one dose, take it as soon as you remember-if it’s within a few hours of the scheduled time. If it’s been longer, skip the missed dose and take your next one at the regular time. Never double up. Missing doses increases rejection risk. If you miss more than one, contact your transplant center immediately. Many centers have 24/7 hotlines for this exact situation.
What Comes Next?
The journey doesn’t end with the transplant. It evolves. You’ll learn what works for your body. You’ll find routines that fit. You’ll connect with others who get it. And you’ll keep pushing for better options-because the goal isn’t just survival. It’s living fully, even with the pills, the tests, and the fears.Stay vigilant. Stay informed. And never hesitate to ask your team the hard questions. Your life after transplant is worth the effort.

15 Comments
Donna Packard
December 17, 2025 AT 06:46Thank you for writing this with such care. I’ve been on tacrolimus for eight years now, and no one ever explains how the fatigue feels like your bones are made of wet sand. You’re not lazy-you’re just constantly fighting a war inside your body. I’m alive, and that’s enough for today.
Stay strong, everyone.
Virginia Seitz
December 19, 2025 AT 00:33Me too 🙌 I take 12 pills a day and still smile. Life’s messy but beautiful. 🌻
Sachin Bhorde
December 19, 2025 AT 00:38Yo, just wanna say-generic mycophenolate saved my ass. Cost $15/month vs $400 for Myfortic. But yeah, my GI went nuts for two weeks. Doc said it’s just the fillers, not the active. Tolerated it after a month. If you’re broke, ask for generics. But don’t switch without monitoring. Bloodwork is your BFF.
Also, grapefruit juice = death. I learned that the hard way. ER visit. Don’t be me.
Peter Ronai
December 19, 2025 AT 23:56Let’s be brutally honest: most transplant patients are just lazy about their meds. You think your ‘fatigue’ is from the drugs? Nah. It’s from scrolling TikTok all day while your GFR plummets. I’ve seen 12 patients reject grafts because they skipped doses to ‘feel normal.’ You don’t get to have a new kidney and then act like a teenager with a new car. This isn’t a privilege-it’s a responsibility. And if you’re taking St. John’s wort? You’re not a patient-you’re a liability.
Michael Whitaker
December 20, 2025 AT 18:45As a physician who consults at a major transplant center, I must emphasize that your comment above is dangerously misinformed. The non-adherence rate is not due to laziness-it’s due to cognitive load, depression, polypharmacy fatigue, and lack of socioeconomic support. Many patients juggle three jobs, no insurance, and no family. Calling them ‘liabilities’ is not clinical-it’s cruel. The system fails them long before they do.
Raven C
December 22, 2025 AT 12:04How profoundly infantilizing. To reduce the exquisite, multidimensional suffering of immunosuppressed individuals to a mere failure of discipline is not merely reductive-it is an affront to medical ethics, philosophical nuance, and basic human dignity. One does not ‘choose’ to endure steroid-induced osteoporosis, or moon face, or the existential dread of a missed dose. The burden is not borne in the will-it is imposed by a system that offers survival at the cost of autonomy, and then blames the survivor for not thriving.
Perhaps if the medical establishment invested in psychosocial support as rigorously as it does in drug monitoring, adherence would not be a ‘problem’-but a natural consequence of care.
And as for St. John’s wort? The FDA has issued warnings. The pharmacokinetics are well-documented. It is not moral failure-it is ignorance. And ignorance, dear sir, is the only true liability here.
Steven Lavoie
December 23, 2025 AT 02:05I appreciate both of your perspectives. Chris, your frustration comes from a place of seeing outcomes, but Michael, you’re right-this isn’t just about willpower. I’ve worked with patients who missed doses because their pharmacy ran out, or their bus got canceled, or they were too nauseous to swallow pills after chemo. One woman took her tacrolimus in the middle of the night because she couldn’t sleep and didn’t want to risk forgetting. That’s not laziness. That’s devotion.
And Raven-your point about autonomy? Spot on. We treat these patients like they’re broken machines that need tightening, not humans who’ve been through hell and are still showing up.
Anu radha
December 23, 2025 AT 23:14I am from India. My brother had kidney transplant. He take medicine every day. He feel tired. But he smile. He say, ‘I am lucky.’ I think, all people who take transplant, they are hero. Not lazy. Not problem. Hero.
Jigar shah
December 24, 2025 AT 07:35Interesting perspective. I’m curious-what percentage of transplant recipients in India have access to therapeutic drug monitoring? In the U.S., it’s nearly universal, but in rural India, many rely on generic drugs without regular blood tests. Is adherence monitored differently there? I ask because I’m researching global disparities in post-transplant care.
Sachin Bhorde
December 24, 2025 AT 23:00Good question, Jigar. In India, TDM is rare outside big cities. Most get generic tacrolimus, no labs for 3-6 months. We use clinical signs: tremor, BP spike, low urine output. If they’re alive after 6 months, we assume it’s working. Not ideal, but survival > perfection. We’ve got 1.4B people and 200 transplant centers. You do what you can. Still, we’re getting better. NGOs are helping with subsidized labs now.
Joe Bartlett
December 25, 2025 AT 16:22Blimey, this is all a bit much. We’ve got a national health service here in the UK. No one’s skipping doses because they can’t afford it. You lot in the States are just being dramatic. Take your pills, stop whining, and get on with it.
Marie Mee
December 27, 2025 AT 10:25Did you know the government puts chemicals in the water to make us dependent on these drugs? They want us sick so they can sell us more pills. I saw a guy on YouTube who stopped all meds and his kidney worked fine. They silenced him. The FDA is part of the cover-up. I don't trust anyone anymore. My pills are hidden in a tin buried in my backyard. I only take them when the moon is full.
Salome Perez
December 28, 2025 AT 11:28What strikes me most is how this post-though clinical in tone-becomes a poem of resilience. The numbers are staggering: 20-30% NODAT, 30-50% fracture risk by year 10, 72% chronic fatigue. But behind each statistic is a person who wakes up, swallows their 10 pills, checks their blood pressure, avoids the raw salmon, and still finds joy in a sunrise.
Transplant isn’t a cure. It’s a covenant-with science, with suffering, with hope. And those who live it? They don’t just survive. They teach us what courage looks like when it’s quiet, daily, and unglamorous.
Thank you for naming the invisible work. It matters.
Brooks Beveridge
December 29, 2025 AT 04:03Salome, you just said what I’ve been trying to articulate for years. This isn’t about compliance. It’s about courage.
I used to be a transplant coordinator. I watched a 19-year-old girl, post-liver transplant, paint her nails every Sunday-even when she was too tired to stand. She said, ‘If I can’t feel my body, I’ll at least make it pretty.’
That’s the real win. Not the GFR. Not the lab results. The fact that someone still chooses to paint their nails.
You’re not just surviving. You’re creating beauty in the wreckage. And that? That’s the most powerful medicine of all.
Naomi Lopez
December 29, 2025 AT 04:27Honestly? I think the real tragedy isn’t the side effects. It’s that we’ve normalized this. We call it ‘the price of life’ like it’s fair. What if we invested in xenotransplantation or bioengineered organs instead of just tweaking immunosuppressants? We’re treating symptoms while ignoring the root. This is medical stagnation dressed up as progress.