Esophageal Varices: Causes, Risks, and What You Need to Know
When you have esophageal varices, enlarged, fragile veins in the lower part of the esophagus that can rupture and cause life-threatening bleeding. Also known as esophageal venous varices, they’re not a disease on their own—they’re a warning sign that something serious is wrong with your liver. These veins swell because blood can’t flow normally through the liver, so it backs up into smaller vessels nearby. The result? Thin-walled, bulging veins that can burst without warning.
This usually happens because of portal hypertension, high blood pressure in the portal vein that carries blood from the intestines to the liver. The most common cause? cirrhosis, scarring of the liver from long-term damage. Alcohol abuse, hepatitis B or C, fatty liver disease—these all lead to cirrhosis over time. Once the liver hardens, it blocks blood flow. That’s when the veins in your esophagus start stretching like overfilled balloons. About 50% of people with cirrhosis develop esophageal varices, and up to 30% of them will bleed at some point.
What makes esophageal varices so dangerous isn’t just that they’re swollen—it’s that they’re silent. You might feel fine until you suddenly vomit blood or pass dark, tarry stools. There’s no pain, no warning. That’s why doctors screen people with advanced liver disease using endoscopy. If varices are found, they can be treated before they bleed. Treatments include beta-blockers to lower pressure, banding to tie off the veins, or in severe cases, a TIPS procedure to reroute blood flow.
It’s not just about the liver. Other conditions like blood clots in the portal vein or rare infections can also cause portal hypertension and lead to varices. But if you’ve been told you have cirrhosis, or you’ve been told your liver enzymes are high, don’t ignore it. Esophageal varices are one of the most serious complications—and they’re preventable if caught early.
Below, you’ll find real, practical articles that explain how these veins form, what doctors do to stop them from bleeding, how medications like beta-blockers help, and why managing your liver health isn’t optional—it’s life-saving. These aren’t theoretical guides. They’re based on what actually works in clinics and emergency rooms.
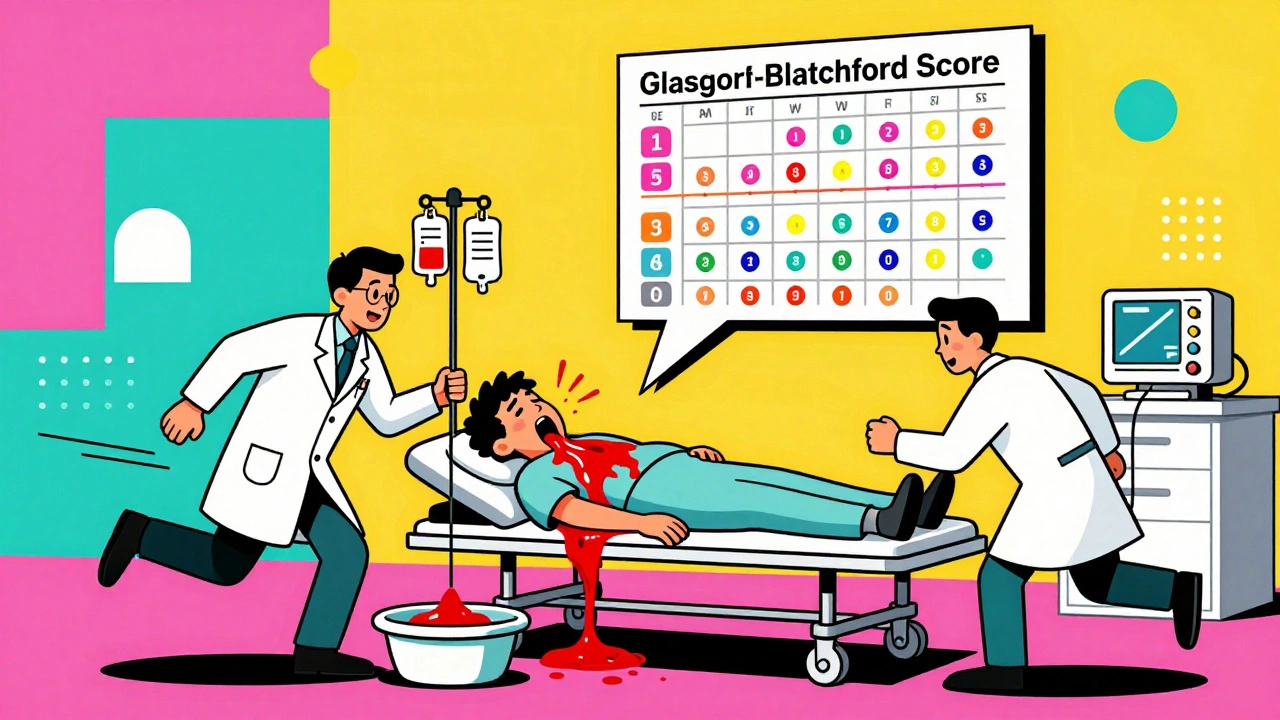
Upper GI Bleeding: Ulcers, Varices, and Stabilization
Upper GI bleeding is a life-threatening emergency caused by ulcers, varices, or other damage to the upper digestive tract. Learn the signs, causes, and life-saving stabilization steps used in modern medicine.
© 2026. All rights reserved.