Alcohol and Opioid Risk Calculator
This tool calculates your risk of respiratory depression based on the alcohol and opioid combination. According to FDA data, mixing alcohol and opioids can be fatal even with small amounts. The risk isn't theoretical—it's been proven in thousands of overdose deaths.
Risk Assessment Result
When you mix alcohol and opioids, you're not just doubling the risk-you're creating a chemical trap that can shut down your breathing without warning. This isn't speculation. It's science. And it's killing people every day.
Why This Combination Is So Dangerous
Both alcohol and opioids slow down your central nervous system. That’s why they make you feel relaxed, drowsy, or even euphoric. But when they’re together, they don’t just add up-they multiply. This synergy hits your brainstem, the part that controls automatic functions like breathing. The result? Your breaths become shallow, infrequent, or stop entirely. The U.S. Food and Drug Administration (FDA) issued a black-box warning in 2016-its strongest safety alert-requiring all prescription opioid labels to explicitly say: do not mix with alcohol. This wasn’t a formality. It was a life-or-death notice backed by data showing alcohol was involved in 15-20% of all opioid-related deaths. A 2017 study in the Journal of Clinical Psychopharmacology found that 20mg of oxycodone alone reduced breathing by 28%. Add just enough alcohol to reach a blood alcohol concentration (BAC) of 0.1%-the legal limit for driving in most U.S. states-and breathing dropped another 19%. Apnea episodes (complete pauses in breathing) spiked, especially in older adults. That’s not a high dose. That’s a standard prescription.Who’s Most at Risk
It’s not just people who misuse drugs. Many who take opioids legally for chronic pain also drink socially. They don’t think it’s a big deal. But the risk starts at low levels. A single glass of wine with a nightly pain pill can be enough to tip the balance. Men are disproportionately affected. Texas data from 2010-2019 showed 77% of alcohol-opioid deaths were among males. But women aren’t safe either. Their bodies process alcohol differently, and even smaller amounts can increase overdose risk. People on methadone maintenance therapy face especially high danger. Research in the journal Addiction found those who drank alcohol while on methadone had 4.6 times the risk of fatal overdose compared to those who didn’t. That’s not a small increase. That’s a near-fivefold jump.Which Opioids Are the Worst?
Not all opioids carry the same risk when mixed with alcohol-but most still do. Prescription opioids like hydrocodone (Vicodin), oxycodone (OxyContin), and fentanyl are the most common culprits. Fentanyl, even in tiny amounts, is especially deadly when combined with alcohol. Synthetic opioids saw the steepest rise in alcohol co-involvement. In Texas, alcohol was found in 9% of fentanyl-related deaths in 2010. By 2019, that number jumped to 17%. Heroin deaths also frequently involved alcohol, with rates hovering between 13% and 20% over the same decade. Even buprenorphine-a medication used to treat opioid use disorder-becomes more dangerous with alcohol. University of Florida researchers found alcohol was present in 30% of fatal buprenorphine overdoses. That’s not a coincidence. Alcohol lowers the threshold for toxicity.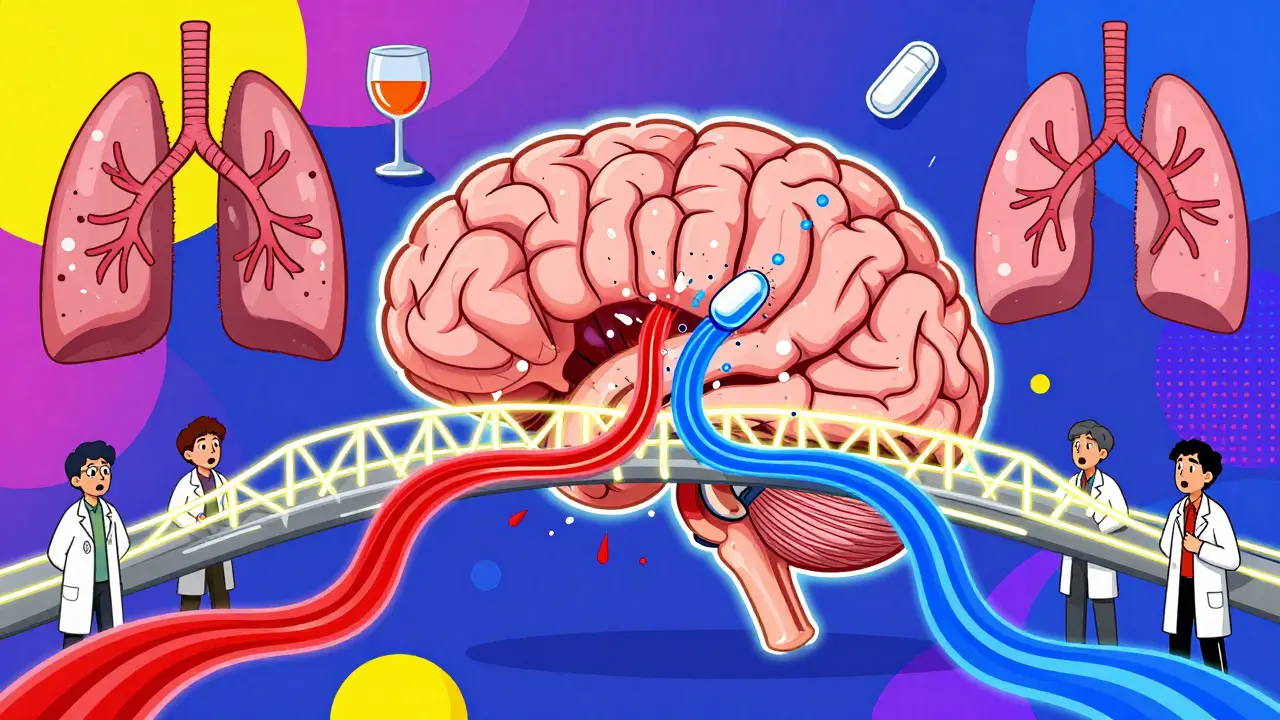
The Bigger Picture: A Public Health Crisis
In 2022, over 107,941 drug overdose deaths occurred in the U.S. Nearly 81% of them involved more than one substance. Alcohol and opioids were one of the most common-and deadliest-combinations. The CDC reports that almost half of all opioid overdoses in 2016 included alcohol, cocaine, or benzodiazepines. Now imagine adding all three together. That’s a triple threat. The National Institute on Drug Abuse (NIDA) found that nearly 14% of opioid deaths in 2021 involved benzodiazepines too. Mix in alcohol, and the risk becomes almost impossible to predict. Worldwide, the World Health Organization (WHO) says over 118,000 people died from opioid overdoses in 2021. Alcohol co-ingestion was a major factor in many of those cases. Respiratory depression-the physical shutdown of breathing-is the leading cause of death. And alcohol makes it happen faster, deeper, and without warning.What Doctors Are Doing About It
Healthcare providers are being forced to change how they prescribe. The American Society of Addiction Medicine (ASAM) now requires doctors to screen for alcohol use disorder before writing an opioid prescription. Patients with alcohol use disorder are 3.2 times more likely to overdose on opioids, according to national survey data. The FDA specifically warns against prescribing opioid cough medicines to anyone taking alcohol or other depressants. That’s because even over-the-counter cough syrups with codeine can be deadly when mixed with a beer or two. Harm reduction efforts are expanding. The CDC recommends naloxone be given to anyone using both alcohol and opioids. In Massachusetts, 23% of naloxone reversals in 2022 involved polysubstance use including alcohol. That means naloxone is saving lives-but only if it’s available when needed.Why People Keep Mixing Them
It’s not always about addiction. Many people take opioids for chronic pain and drink to relax after work. Others use alcohol to cope with opioid withdrawal symptoms. Some don’t even realize the danger. A 2014 study found that nearly 40% of patients prescribed opioids didn’t know they should avoid alcohol. Pharmaceutical companies have been sued for downplaying these risks. Purdue Pharma’s $6 billion settlement in 2023 included funding for alcohol screening programs for opioid patients. That’s a sign of how deeply this problem is rooted in systemic failures.What You Can Do
If you or someone you know takes opioids-even legally-do not drink alcohol. Not even one drink. Not even on special occasions. The risk isn’t worth it. If you’re on methadone or buprenorphine, talk to your doctor about alcohol use. Don’t hide it. Your life depends on honesty. If you’re using opioids recreationally, carry naloxone. Know how to use it. Teach your friends how to use it too. Naloxone can reverse an opioid overdose-but it won’t help if you’ve also mixed in alcohol. Emergency services are still needed.The Future: New Tools, Same Danger
There’s hope. In June 2023, researchers at the University of Pittsburgh identified a potential early warning sign: reduced heart rate variability. This biomarker predicted 83% of alcohol-opioid overdose cases 30 minutes before breathing stopped. Future wearable tech could alert users before it’s too late. The Substance Abuse and Mental Health Services Administration (SAMHSA) launched the ‘Don’t Mix’ campaign in January 2023 with $15 million in funding. Their goal? A 10% drop in co-involved overdoses by 2025. But without major changes in prescribing, education, and access to treatment, the CDC predicts alcohol-opioid deaths will rise 7.2% each year through 2025. That’s not a trend. That’s a countdown.Final Reality Check
You don’t need to be an addict to die from mixing alcohol and opioids. You just need to believe it’s safe. It’s not. The data doesn’t lie. The warnings aren’t exaggerations. The deaths are real-and preventable. If you’re taking opioids, skip the drink. If you’re drinking, don’t take the pill. There’s no safe middle ground. The combination is lethal. Period.Can you die from mixing alcohol and opioids even if you take them as prescribed?
Yes. Even when taken exactly as directed by a doctor, combining alcohol with prescription opioids like oxycodone or hydrocodone can cause fatal respiratory depression. The FDA’s black-box warning exists because this risk isn’t theoretical-it’s been proven in thousands of overdose deaths. A single drink can be enough to push the body past its limit, especially in older adults or those with underlying health conditions.
How long should I wait after taking an opioid before drinking alcohol?
You shouldn’t drink alcohol at all if you’re taking opioids. There’s no safe waiting period. Even long-acting opioids like OxyContin or fentanyl patches stay in your system for hours or days. Alcohol affects your brain and liver continuously, and the interaction isn’t just about timing-it’s about cumulative suppression of breathing. No amount of waiting eliminates the risk.
Does naloxone work if someone overdoses on alcohol and opioids together?
Naloxone can reverse the opioid component of the overdose, but it does nothing for alcohol. If someone has mixed both substances, naloxone may bring them back temporarily, but alcohol will continue to depress their breathing. Emergency medical help is still absolutely necessary. Naloxone saves lives-but it’s not a cure-all when alcohol is involved.
Is it safer to use alcohol with non-prescription opioids like heroin or fentanyl?
No. In fact, it’s even more dangerous. Illicit opioids like fentanyl are often much stronger and more unpredictable than prescription versions. Mixing them with alcohol dramatically increases the chance of sudden, fatal respiratory failure. Toxicology reports show alcohol is present in nearly half of all fentanyl-related deaths. There is no safe way to combine them.
Can alcohol make opioid withdrawal worse?
Yes. While some people drink to ease withdrawal symptoms like anxiety or insomnia, alcohol actually worsens them over time. It disrupts sleep, increases anxiety, and puts extra stress on the liver and nervous system. Using alcohol during withdrawal can lead to rebound cravings, increased risk of relapse, and dangerous interactions if opioids are taken again. Medical supervision is critical during detox.
Are there any medications that are safe to take with alcohol if you’re on opioids?
No. Any medication that depresses the central nervous system-sleep aids, anti-anxiety drugs, muscle relaxants, or even some antihistamines-should be avoided with both alcohol and opioids. The combination can lead to the same deadly outcome: slowed or stopped breathing. Always check with your doctor or pharmacist before taking any new medication or supplement while on opioids.

